Risk factors and outcome of COVID-19 in patients with hematological malignancies
José Luis Piñana, Rodrigo Martino, Irene García-García, Rocío Parody, María Dolores Morales, Gonzalo Benzo, Irene Gómez-Catalan, Rosa Coll, Ignacio De La Fuente, Alejandro Luna, Beatriz Merchán, Anabelle Chinea, Dunia De Miguel, Ana Serrano, Carmen Pérez, Carola Diaz, José Luis Lopez, Adolfo Jesús Saez, Rebeca Bailen, Teresa Zudaire, Diana Martínez, Manuel Jurado, María Calbacho, Lourdes Vázquez, Irene Garcia-Cadenas, Laura Fox, Ana I Pimentel, Guiomar Bautista, Agustin Nieto, Pascual Fernandez, Juan Carlos Vallejo, Carlos Solano, Marta Valero, Ildefonso Espigado, Raquel Saldaña, Luisa Sisinni, Josep Maria Ribera, Maria Jose Jimenez, Maria Trabazo, Marta Gonzalez-Vicent, Noemí Fernández, Carme Talarn, Maria Carmen Montoya, Angel Cedillo, Anna Sureda
Experimental Hematology & Oncology, doi:10.1186/s40164-020-00177-z
Background: Prognostic factors of poor outcome in patients with hematological malignancies and COVID-19 are poorly defined.
Patients and methods: This was a Spanish transplant group and cell therapy (GETH) multicenter retrospective observational study, which included a large cohort of blood cancer patients with laboratory-confirmed SARS-CoV-2 infection through PCR assays from March 1st 2020 to May 15th 2020.
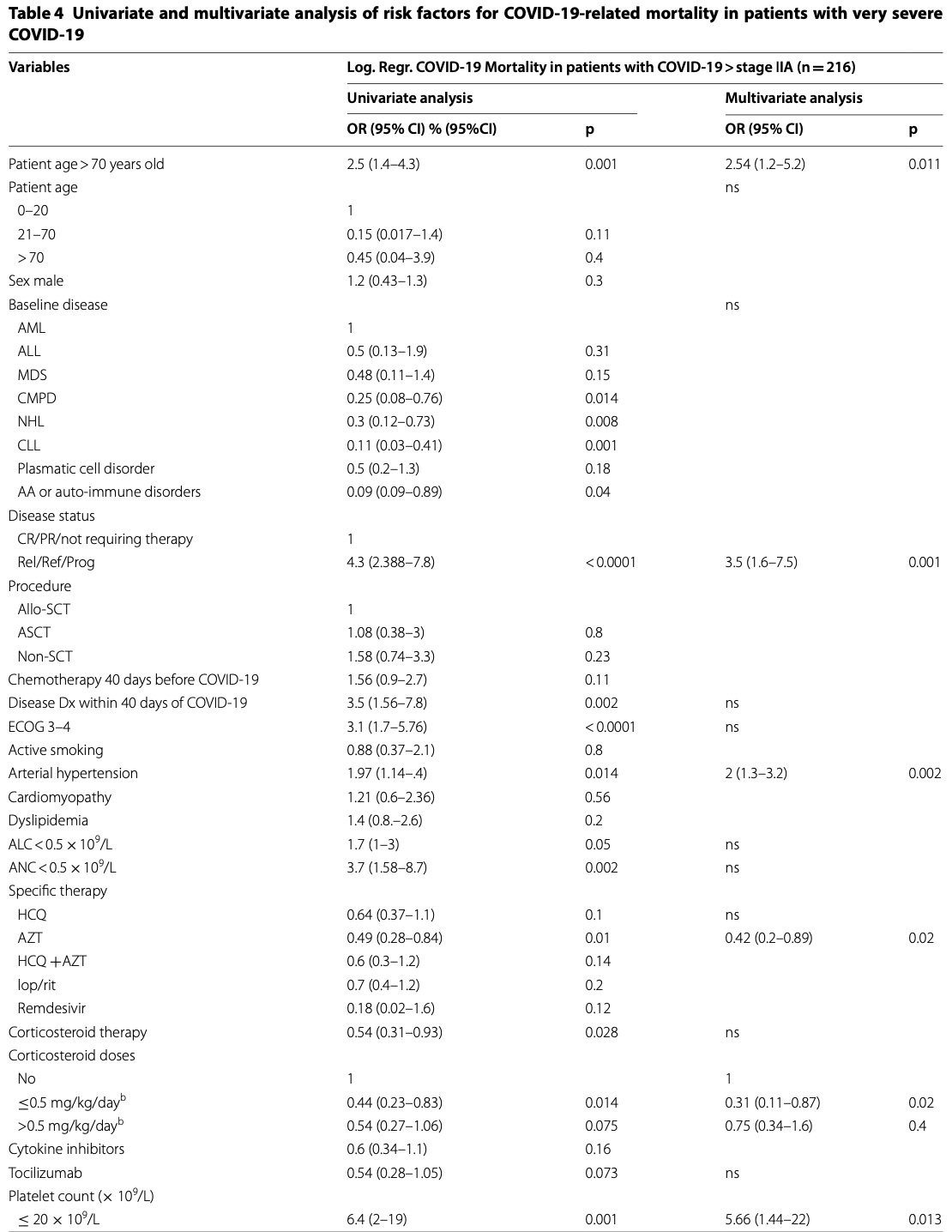
Results: We included 367 pediatric and adult patients with hematological malignancies, including recipients of autologous (ASCT) (n = 58) or allogeneic stem cell transplantation (allo-SCT) (n = 65) from 41 hospitals in Spain. Median age of patients was 64 years (range 1-93.8). Recipients of ASCT and allo-SCT showed lower mortality rates (17% and 18%, respectively) compared to non-SCT patients (31%) (p = 0.02). Prognostic factors identified for day 45 overall mortality (OM) by logistic regression multivariate analysis included age > 70 years [odds ratio (OR) 2.1, 95% confidence interval (CI) 1.2-3.8, p = 0.011]; uncontrolled hematological malignancy (OR 2.9, 95% CI 1.6-5.2, p < 0.0001); ECOG 3-4 (OR, 2.56, 95% CI 1.4-4.7, p = 0.003); neutropenia (< 0.5 × 10 9 /L) (OR 2.8, 95% CI 1.3-6.1, p = 0.01); and a C-reactive protein (CRP) > 20 mg/dL (OR 3.3, p < 0.0001). In multivariate analysis of 216 patients with very severe COVID-19, treatment with azithromycin or low dose corticosteroids was associated with lower OM (OR 0.42, 95% CI 0.2-0.89 and OR 0.31, 95% CI 0.11-0.87, respectively, p = 0.02) whereas the use of hidroxycloroquine did not show significant improvement in OM (OR 0.64, 95% CI 0.37-1.1, P = 0.1).
Authors' contributions JLP, and RM designed the study and drafted the manuscript. All authors participated in the revision of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate All patients gave their informed consent. Local ethics committee approved the study protocol (reference code 2020-113-1), registered by the Spanish Agency of Medicines and Health Products with the reference code GET-CLO-2020-01 and by the European Medicines Agency with the reference code EUPAS34365EBMT.
Consent for publication The participants provided informed consent for the publication of the study.
Competing interests The author(s) declare that they have no conflict of interests. Author details Piñana et al. Exp Hematol Oncol (2020) 9:21 • thorough peer review by experienced researchers in your field • rapid publication on acceptance • support for research data, including large and complex data types • gold Open Access which fosters wider collaboration and increased citations maximum visibility for your research: over 100M website views per year
• At BMC, research is always in progress.
Learn more biomedcentral.com/submissions Ready to submit your research ? Choose BMC and benefit from: es-death -by-up-to-one-third -in-hospi talis ed-patie nts-with-sever e-respi rator y-compl icati ons-of-covid -
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional..
References
Arons, Hatfield, Reddy, Kimball, James et al., Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility, N Engl J Med
Bhargava, Fukushima, Levine, Zhao, Tanveer et al., Predictors for severe COVID-19 infection, Clin Infect Dis,
doi:10.1093/cid/ciaa674Chen, Zheng, Liu, Yan, Xu et al., Plasma CRP level is positively associated with the severity of COVID-19, Ann Clin Microbiol Antimicrob
Cheson, Fisher, Barrington, Cavalli, Schwartz et al., Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study Group; German Hodgkin's Study Group; Japanese Lymphorra Study Group; Lymphoma Study Association, J Clin Oncol
Chien, Martin, Gooley, Flowers, Heckbert et al., Airflow obstruction after myeloablative allogeneic hematopoietic stem cell transplantation, Am J Respir Crit Care Med
Dai, Liu, Liu, Zhou, Li et al., Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak, Cancer Discov,
doi:10.1158/2159-8290.cd-20-0422Döhner, Estey, Grimwade, Amadori, Appelbaum et al., Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel, Blood,
doi:10.1182/blood-2016-08-733196Erard, Chien, Kim, Nichols, Flowers et al., Airflow decline after myeloablative allogeneic hematopoietic cell transplantation: the role of community respiratory viruses, J Infect Dis
Fadel, Morrison, Vahia, Smith, Chaudhry et al., Henry Ford COVID-19 Management Task Force Early short course corticosteroids in hospitalized patients with COVID-19, Clin Infect Dis,
doi:10.1093/cid/ciaa601Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Hao, Lian, Lu, Jia, Hu et al., Decreased B cells on admission was associated with prolonged viral RNA shedding from respiratory tract in Coronavirus Disease 2019: a case control study, J Infect Dis,
doi:10.1093/infdis/jiaa311Hoffmann, Kleine-Weber, Schroeder, Kruger, Herrler et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell,
doi:10.1016/j.cell.2020.02.052Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Jing, Ya, Xi, Pu, Zhaofeng et al., Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis, Int J Infect Dis,
doi:10.1016/j.ijid.2020.03.017Kolilekas, Loverdos, Giannakaki, Vlassi, Levounets et al., Can steroids reverse the severe COVID-19 induced 'cytokine storm, J Med Virol,
doi:10.1002/jmv.26165Kuderer, Choueiri, Shah, Shyr, Rubinstein et al., COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study, Lancet,
doi:10.1016/s0140-6736(20)31187-9Kumar, Paiva, Anderson, Durie, Landgren et al., International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma, Lancet Oncol,
doi:10.1016/S1470-2045(16)30206-6Lapostolle, Schneider, Vianu, Dollet, Roche et al., Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: the COVIDcall study, Intern Emerg Med,
doi:10.1007/s11739-020-02379-zLiang, Guan, Chen, Li, Xu et al., Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China, Lancet Oncol
Malard, Genthon, Brissot, Van De Wyngaert, Marjanovic et al., COVID-19 outcomes in patients with hematologic disease, Bone Marrow Transplant,
doi:10.1038/s41409-020-0931-4Martín-Moro, Marquet, Piris, Michael, Sáez et al., Survival study of hospitalised patients with concurrent COVID-19 and haematological malignancies, Br J Haematol,
doi:10.1111/bjh.16801Miyashita, Mikami, Chopra, Yamada, Chernyavsky et al., Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City, Ann Oncol,
doi:10.1016/j.annonc.2020.04.006Nishiura, Kobayashi, Miyama, Suzuki, Jung et al., Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19), Int J Infect Dis
Oken, Creech, Tormey, Horton, Davis et al., Toxicity and response criteria of the Eastern Cooperative Oncology Group, Am J Clin Oncol
Piñana, Pérez, Montoro, Hernani, Lorenzo et al., The effect of timing on community acquired respiratory virus infection mortality during the first year after allogeneic hematopoietic stem cell transplantation: a prospective epidemiological survey, Bone Marrow Transplant
Rosenberg, Dufort, Udo, Wilberschied, Kumar et al., Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State, JAMA,
doi:10.1001/jama.2020.8630Scarfò, Chatzikonstantinou, Rigolin, Quaresmini, Motta et al., COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus, Leukemia,
doi:10.1038/s41375-020-0959-xShah, Ghantoji, Mulanovich, Ariza-Heredia, Chemaly, Management of respiratory viral infections in hematopoietic cell transplant recipients, Am J Blood Res
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal, J Heart Lung Transplant
So, Ro, Murakami, Imai, Jinta, High-dose, short-term corticosteroids for ARDS caused by COVID-19: a case series, Respirol Case Rep
Vikas, Sanjay, Rafi, Daniel, Mendel et al., Case fatality rate of cancer patients with COVID-19 in a New York Hospital System, Cancer Discov,
doi:10.1158/2159-8290.CD-20-0516Wan, Xiang, Fang, Zheng, Li et al., Clinical features and treatment of COVID-19 patients in northeast Chongqing, J Med Virol
Wang, Van Oekelen, Mouhieddine, Valle, Richter et al., A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward, J Hematol Oncol
Wu, Chen, Cai, Xia, Zhou et al., Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China, JAMA Internal Medicine,
doi:10.1001/jamainternmed.2020.0994Wu, Chen, Cai, Xia, Zhou et al., Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China, JAMA Intern Med
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention, JAMA,
doi:10.1001/jama.2020.2648Yang, Liu, Zhou, Zhao, Zhao et al., The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis, J Infect
Yang, Yu, Xu, Shu, Liu et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med,
doi:10.1016/S2213-2600(20)30079-5Yuan, Xu, Xia, Tao, Yin et al., Effects of corticosteroid treatment for non-severe COVID-19 pneumonia: a propensity score-based analysis, Shock,
doi:10.1097/SHK.0000000000001574Zhang, Dong, Cao, Yuan, Yang et al., Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China, Allergy,
doi:10.1111/all.14238Zhou, Yang, Wang, Hu, Zhang et al., A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zou, Ruan, Huang, SARS-CoV-2 viral load in upper respiratory specimens of infected patients, N Engl J Med
DOI record:
{
"DOI": "10.1186/s40164-020-00177-z",
"ISSN": [
"2162-3619"
],
"URL": "http://dx.doi.org/10.1186/s40164-020-00177-z",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Background</jats:title><jats:p>Prognostic factors of poor outcome in patients with hematological malignancies and COVID-19 are poorly defined.</jats:p></jats:sec><jats:sec><jats:title>Patients and methods</jats:title><jats:p>This was a Spanish transplant group and cell therapy (GETH) multicenter retrospective observational study, which included a large cohort of blood cancer patients with laboratory-confirmed SARS-CoV-2 infection through PCR assays from March 1st 2020 to May 15th 2020.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>We included 367 pediatric and adult patients with hematological malignancies, including recipients of autologous (ASCT) (n = 58) or allogeneic stem cell transplantation (allo-SCT) (n = 65) from 41 hospitals in Spain. Median age of patients was 64 years (range 1–93.8). Recipients of ASCT and allo-SCT showed lower mortality rates (17% and 18%, respectively) compared to non-SCT patients (31%) (p = 0.02). Prognostic factors identified for day 45 overall mortality (OM) by logistic regression multivariate analysis included age > 70 years [odds ratio (OR) 2.1, 95% confidence interval (CI) 1.2–3.8, p = 0.011]; uncontrolled hematological malignancy (OR 2.9, 95% CI 1.6–5.2, p < 0.0001); ECOG 3–4 (OR, 2.56, 95% CI 1.4–4.7, p = 0.003); neutropenia (< 0.5 × 10<jats:sup>9</jats:sup>/L) (OR 2.8, 95% CI 1.3–6.1, p = 0.01); and a C-reactive protein (CRP) > 20 mg/dL (OR 3.3, 95% CI 1.7–6.4, p < 0.0001). In multivariate analysis of 216 patients with very severe COVID-19, treatment with azithromycin or low dose corticosteroids was associated with lower OM (OR 0.42, 95% CI 0.2–0.89 and OR 0.31, 95% CI 0.11–0.87, respectively, p = 0.02) whereas the use of hidroxycloroquine did not show significant improvement in OM (OR 0.64, 95% CI 0.37–1.1, P = 0.1).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>In most patients with hematological malignancies COVID-19 mortality was directly driven by older age, disease status, performance status, as well as by immune (neutropenia) parameters and level of inflammation (high CRP). Use of azithromycin and low dose corticosteroids may be of value in very severe COVID-19.</jats:p></jats:sec>",
"alternative-id": [
"177"
],
"article-number": "21",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "16 July 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "18 August 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "25 August 2020"
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "All patients gave their informed consent. Local ethics committee approved the study protocol (reference code 2020-113-1), registered by the Spanish Agency of Medicines and Health Products with the reference code GETCLO-2020-01 and by the European Medicines Agency with the reference code EUPAS34365EBMT."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The participants provided informed consent for the publication of the study."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The author(s) declare that they have no conflict of interests."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-8533-2562",
"affiliation": [],
"authenticated-orcid": false,
"family": "Piñana",
"given": "José Luis",
"sequence": "first"
},
{
"affiliation": [],
"family": "Martino",
"given": "Rodrigo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "García-García",
"given": "Irene",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parody",
"given": "Rocío",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morales",
"given": "María Dolores",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Benzo",
"given": "Gonzalo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gómez-Catalan",
"given": "Irene",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Coll",
"given": "Rosa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "De La Fuente",
"given": "Ignacio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Luna",
"given": "Alejandro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Merchán",
"given": "Beatriz",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chinea",
"given": "Anabelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Miguel",
"given": "Dunia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Serrano",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pérez",
"given": "Carmen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Diaz",
"given": "Carola",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lopez",
"given": "José Luis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saez",
"given": "Adolfo Jesús",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bailen",
"given": "Rebeca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zudaire",
"given": "Teresa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Martínez",
"given": "Diana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jurado",
"given": "Manuel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Calbacho",
"given": "María",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vázquez",
"given": "Lourdes",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Garcia-Cadenas",
"given": "Irene",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fox",
"given": "Laura",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pimentel",
"given": "Ana I.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bautista",
"given": "Guiomar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nieto",
"given": "Agustin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fernandez",
"given": "Pascual",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vallejo",
"given": "Juan Carlos",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Solano",
"given": "Carlos",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Valero",
"given": "Marta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Espigado",
"given": "Ildefonso",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saldaña",
"given": "Raquel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sisinni",
"given": "Luisa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ribera",
"given": "Josep Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jimenez",
"given": "Maria Jose",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Trabazo",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gonzalez-Vicent",
"given": "Marta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fernández",
"given": "Noemí",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Talarn",
"given": "Carme",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Montoya",
"given": "Maria Carmen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cedillo",
"given": "Angel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sureda",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [],
"name": "Infectious Complications Subcommittee of the Spanish Hematopoietic Stem Cell Transplantation and Cell Therapy Group (GETH)",
"sequence": "additional"
}
],
"container-title": "Experimental Hematology & Oncology",
"container-title-short": "Exp Hematol Oncol",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2020,
8,
25
]
],
"date-time": "2020-08-25T12:02:43Z",
"timestamp": 1598356963000
},
"deposited": {
"date-parts": [
[
2023,
10,
6
]
],
"date-time": "2023-10-06T07:56:15Z",
"timestamp": 1696578975000
},
"indexed": {
"date-parts": [
[
2024,
2,
23
]
],
"date-time": "2024-02-23T14:26:50Z",
"timestamp": 1708698410748
},
"is-referenced-by-count": 109,
"issue": "1",
"issued": {
"date-parts": [
[
2020,
8,
25
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2020,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
8,
25
]
],
"date-time": "2020-08-25T00:00:00Z",
"timestamp": 1598313600000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
8,
25
]
],
"date-time": "2020-08-25T00:00:00Z",
"timestamp": 1598313600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s40164-020-00177-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s40164-020-00177-z/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s40164-020-00177-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2020,
8,
25
]
]
},
"published-online": {
"date-parts": [
[
2020,
8,
25
]
]
},
"published-print": {
"date-parts": [
[
2020,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"author": "W Guan",
"doi-asserted-by": "publisher",
"first-page": "1708",
"journal-title": "N Engl J Med",
"key": "177_CR1",
"unstructured": "Guan W, Ni Z, Yu Hu, Liang W, Ou C, He J, Liu L, Shan H, Lei C, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20.",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"author": "X Yang",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Respir Med.",
"key": "177_CR2",
"unstructured": "Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020. https://doi.org/10.1016/S2213-2600(20)30079-5.",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Lancet",
"key": "177_CR3",
"unstructured": "Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"author": "Jing Yang",
"doi-asserted-by": "publisher",
"journal-title": "Int J Infect Dis",
"key": "177_CR4",
"unstructured": "Yang Jing, Zheng Ya, Gou Xi, Ke Pu, Chen Zhaofeng, Guo Qinghong, Ji Rui, Wang Haojia, Wang Yuping, Zhou Yongning. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020. https://doi.org/10.1016/j.ijid.2020.03.017.",
"year": "2020"
},
{
"DOI": "10.1164/rccm.200212-1468OC",
"author": "JW Chien",
"doi-asserted-by": "publisher",
"first-page": "208",
"issue": "2",
"journal-title": "Am J Respir Crit Care Med",
"key": "177_CR5",
"unstructured": "Chien JW, Martin PJ, Gooley TA, Flowers ME, Heckbert SR, Nichols WG, Clark JG. Airflow obstruction after myeloablative allogeneic hematopoietic stem cell transplantation. Am J Respir Crit Care Med. 2003;168(2):208–14.",
"volume": "168",
"year": "2003"
},
{
"DOI": "10.1086/504268",
"author": "V Erard",
"doi-asserted-by": "publisher",
"first-page": "1619",
"issue": "12",
"journal-title": "J Infect Dis",
"key": "177_CR6",
"unstructured": "Erard V, Chien JW, Kim HW, Nichols WG, Flowers ME, Martin PJ, Corey L, Boeckh M. Airflow decline after myeloablative allogeneic hematopoietic cell transplantation: the role of community respiratory viruses. J Infect Dis. 2006;193(12):1619–25.",
"volume": "193",
"year": "2006"
},
{
"DOI": "10.1016/S1470-2045(20)30096-6",
"author": "W Liang",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "Lancet Oncol",
"key": "177_CR7",
"unstructured": "Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–7.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1158/2159-8290.cd-20-0422",
"author": "M Dai",
"doi-asserted-by": "publisher",
"journal-title": "Cancer Discov",
"key": "177_CR8",
"unstructured": "Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, Zhang Z, You H, Wu M, Zheng Q, et al. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020. https://doi.org/10.1158/2159-8290.cd-20-0422(published online April 28).",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.04.006",
"author": "H Miyashita",
"doi-asserted-by": "publisher",
"journal-title": "Ann Oncol",
"key": "177_CR9",
"unstructured": "Miyashita H, Mikami T, Chopra N, Yamada T, Chernyavsky S, Rizk D, Cruz C. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol. 2020. https://doi.org/10.1016/j.annonc.2020.04.006(published online April 21).",
"year": "2020"
},
{
"DOI": "10.1038/s41409-020-0931-4",
"author": "F Malard",
"doi-asserted-by": "publisher",
"journal-title": "Bone Marrow Transplant",
"key": "177_CR10",
"unstructured": "Malard F, Genthon A, Brissot E, van de Wyngaert Z, Marjanovic Z, Ikhlef S, Banet A, Lapusan S, Sestilli S, Corre E, et al. COVID-19 outcomes in patients with hematologic disease. Bone Marrow Transplant. 2020. https://doi.org/10.1038/s41409-020-0931-4.",
"year": "2020"
},
{
"DOI": "10.1111/bjh.16801",
"author": "F Martín-Moro",
"doi-asserted-by": "publisher",
"journal-title": "Br J Haematol",
"key": "177_CR11",
"unstructured": "Martín-Moro F, Marquet J, Piris M, Michael BM, Sáez AJ, Corona M, Jiménez C, Astibia B, García I, Rodríguez E, et al. Survival study of hospitalised patients with concurrent COVID-19 and haematological malignancies. Br J Haematol. 2020. https://doi.org/10.1111/bjh.16801.",
"year": "2020"
},
{
"DOI": "10.1038/s41375-020-0959-x",
"author": "L Scarfò",
"doi-asserted-by": "publisher",
"journal-title": "Leukemia",
"key": "177_CR12",
"unstructured": "Scarfò L, Chatzikonstantinou T, Rigolin GM, Quaresmini G, Motta M, Vitale C, Garcia-Marco JA, Hernández-Rivas JÁ, Mirás F, Baile M, et al. COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus. Leukemia. 2020. https://doi.org/10.1038/s41375-020-0959-x.",
"year": "2020"
},
{
"DOI": "10.1158/2159-8290.CD-20-0516",
"author": "Vikas Mehta",
"doi-asserted-by": "publisher",
"first-page": "935",
"issue": "7",
"journal-title": "Cancer Discov",
"key": "177_CR13",
"unstructured": "Mehta Vikas, Goel Sanjay, Kabarriti Rafi, Cole Daniel, Goldfinger Mendel, Acuna-Villaorduna Ana, Pradhan Kith, Thota Raja, Reissman Stan, Sparano Joseph A, et al. Case fatality rate of cancer patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020;10(7):935–41. https://doi.org/10.1158/2159-8290.CD-20-0516.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1186/s13045-020-00934-x",
"author": "B Wang",
"doi-asserted-by": "publisher",
"first-page": "94",
"journal-title": "J Hematol Oncol",
"key": "177_CR14",
"unstructured": "Wang B, Van Oekelen O, Mouhieddine TH, Del Valle DM, Richter J, Cho HJ, Richard S, Chari A, Gnjatic S, Merad M, et al. A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward. J Hematol Oncol. 2020;13:94.",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"author": "HK Siddiqi",
"doi-asserted-by": "publisher",
"first-page": "405",
"journal-title": "J Heart Lung Transplant",
"key": "177_CR15",
"unstructured": "Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical–therapeutic staging proposal. J Heart Lung Transplant. 2020;39:405–7.",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1182/blood-2016-08-733196",
"author": "H Döhner",
"doi-asserted-by": "publisher",
"first-page": "424",
"issue": "4",
"journal-title": "Blood",
"key": "177_CR16",
"unstructured": "Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47. https://doi.org/10.1182/blood-2016-08-733196.",
"volume": "129",
"year": "2017"
},
{
"DOI": "10.1200/JCO.2013.54.8800",
"doi-asserted-by": "crossref",
"key": "177_CR17",
"unstructured": "Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, Lister TA; Alliance, Australasian Leukaemia and Lymphoma Group; Eastern Cooperative Oncology Group; European Mantle Cell Lymphoma Consortium; Italian Lymphoma Foundation; European Organisation for Research; Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study Group; German Hodgkin’s Study Group; Japanese Lymphorra Study Group; Lymphoma Study Association; NCIC Clinical Trials Group; Nordic Lymphoma Study Group; Southwest Oncology Group; United Kingdom National Cancer Research Institute. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014 Sep 20;32(27):3059–68."
},
{
"DOI": "10.1016/S1470-2045(16)30206-6",
"author": "S Kumar",
"doi-asserted-by": "publisher",
"first-page": "e328",
"issue": "8",
"journal-title": "Lancet Oncol.",
"key": "177_CR18",
"unstructured": "Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, Munshi N, Lonial S, Bladé J, Mateos MV, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–46. https://doi.org/10.1016/S1470-2045(16)30206-6.",
"volume": "17",
"year": "2016"
},
{
"DOI": "10.1097/00000421-198212000-00014",
"author": "MM Oken",
"doi-asserted-by": "publisher",
"first-page": "649",
"journal-title": "Am J Clin Oncol",
"key": "177_CR19",
"unstructured": "Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.",
"volume": "5",
"year": "1982"
},
{
"DOI": "10.1007/s11739-020-02379-z",
"author": "F Lapostolle",
"doi-asserted-by": "publisher",
"journal-title": "Intern Emerg Med",
"key": "177_CR20",
"unstructured": "Lapostolle F, Schneider E, Vianu I, Dollet G, Roche B, Berdah J, Michel J, Goix L, Chanzy E, Petrovic T, et al. Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: the COVID-call study. Intern Emerg Med. 2020. https://doi.org/10.1007/s11739-020-02379-z(Epub ahead of print).",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa311",
"author": "S Hao",
"doi-asserted-by": "publisher",
"journal-title": "J Infect Dis",
"key": "177_CR21",
"unstructured": "Hao S, Lian J, Lu Y, Jia H, Hu J, Yu G, Wang X, Xu K, Ni Q, Li Y, et al. Decreased B cells on admission was associated with prolonged viral RNA shedding from respiratory tract in Coronavirus Disease 2019: a case control study. J Infect Dis. 2020. https://doi.org/10.1093/infdis/jiaa311(Epub ahead of print).",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25990",
"author": "Y Wang",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol",
"key": "177_CR22",
"unstructured": "Wang Y, Kang H, Liu X, Tong Z. Asymptomatic cases with SARS-CoV-2 infection. J Med Virol. 2020. https://doi.org/10.1002/jmv.25990(Epub ahead of print).",
"year": "2020"
},
{
"DOI": "10.32580/idcr.2020.12.3.17",
"doi-asserted-by": "crossref",
"key": "177_CR23",
"unstructured": "Division of Risk Assessment and International Cooperation. The updates on COVID-19 in Korea as of April 17. Korea Centers for Disease Control & Prevention, 2020."
},
{
"DOI": "10.1016/j.ijid.2020.03.020",
"author": "H Nishiura",
"doi-asserted-by": "publisher",
"first-page": "154",
"journal-title": "Int J Infect Dis.",
"key": "177_CR24",
"unstructured": "Nishiura H, Kobayashi T, Miyama T, Suzuki A, Jung SM, Hayashi K, Kinoshita R, Yang Y, Yuan B, Akhmetzhanov AR, Linton NM. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020;94:154–5.",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2008457",
"author": "MM Arons",
"doi-asserted-by": "publisher",
"first-page": "2081",
"journal-title": "N Engl J Med",
"key": "177_CR25",
"unstructured": "Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, Taylor J, Spicer K, Bardossy AC, Oakley LP, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–90.",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2001737",
"author": "L Zou",
"doi-asserted-by": "publisher",
"first-page": "1177",
"journal-title": "N Engl J Med",
"key": "177_CR26",
"unstructured": "Zou L, Ruan F, Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–9.",
"volume": "382",
"year": "2020"
},
{
"author": "DP Shah",
"first-page": "203",
"issue": "4",
"journal-title": "Am J Blood Res.",
"key": "177_CR27",
"unstructured": "Shah DP, Ghantoji SS, Mulanovich VE, Ariza-Heredia EJ, Chemaly RF. Management of respiratory viral infections in hematopoietic cell transplant recipients. Am J Blood Res. 2012;2(4):203–18 (Epub 2012 Nov 25).",
"volume": "2",
"year": "2012"
},
{
"DOI": "10.1038/s41586-020-2012-7",
"author": "P Zhou",
"doi-asserted-by": "publisher",
"first-page": "270",
"journal-title": "Nature",
"key": "177_CR28",
"unstructured": "Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3.",
"volume": "579",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"author": "M Hoffmann",
"doi-asserted-by": "publisher",
"journal-title": "Cell",
"key": "177_CR29",
"unstructured": "Hoffmann M, Kleine-Weber H, Schroeder S, Kruger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020. https://doi.org/10.1016/j.cell.2020.02.052.",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet",
"key": "177_CR30",
"unstructured": "Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25783",
"author": "S Wan",
"doi-asserted-by": "publisher",
"first-page": "797",
"issue": "7",
"journal-title": "J Med Virol.",
"key": "177_CR31",
"unstructured": "Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, Lang C, Huang D, Sun Q, Xiong Y, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;92(7):797–806.",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1111/all.14238",
"author": "JJ Zhang",
"doi-asserted-by": "publisher",
"journal-title": "Allergy",
"key": "177_CR32",
"unstructured": "Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020. https://doi.org/10.1111/all.14238.",
"year": "2020"
},
{
"DOI": "10.1038/s41409-019-0698-7",
"author": "JL Piñana",
"doi-asserted-by": "publisher",
"first-page": "431",
"issue": "2",
"journal-title": "Bone Marrow Transplant",
"key": "177_CR33",
"unstructured": "Piñana JL, Pérez A, Montoro J, Hernani R, Lorenzo I, Giménez E, Gómez MD, Guerreiro M, González-Barberá EM, Carretero C, et al. The effect of timing on community acquired respiratory virus infection mortality during the first year after allogeneic hematopoietic stem cell transplantation: a prospective epidemiological survey. Bone Marrow Transplant. 2020;55(2):431–40.",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"author": "C Wu",
"doi-asserted-by": "publisher",
"journal-title": "JAMA Internal Medicine.",
"key": "177_CR34",
"unstructured": "Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Internal Medicine. 2020. https://doi.org/10.1001/jamainternmed.2020.0994.",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa674",
"author": "A Bhargava",
"doi-asserted-by": "publisher",
"journal-title": "Clin Infect Dis",
"key": "177_CR35",
"unstructured": "Bhargava A, Fukushima EA, Levine M, Zhao W, Tanveer F, Szpunar SM, Saravolatz L. Predictors for severe COVID-19 infection. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa674.",
"year": "2020"
},
{
"DOI": "10.1186/s12941-020-00362-2",
"author": "W Chen",
"doi-asserted-by": "publisher",
"first-page": "18",
"issue": "1",
"journal-title": "Ann Clin Microbiol Antimicrob.",
"key": "177_CR36",
"unstructured": "Chen W, Zheng KI, Liu S, Yan Z, Xu C, Qiao Z. Plasma CRP level is positively associated with the severity of COVID-19. Ann Clin Microbiol Antimicrob. 2020;19(1):18.",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/s0140-6736(20)31187-9",
"author": "NM Kuderer",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "177_CR37",
"unstructured": "Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, Shete S, Hsu CY, Desai A, de Lima Lopes G Jr, et al. COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020. https://doi.org/10.1016/s0140-6736(20)31187-9.",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"author": "Z Wu",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "177_CR38",
"unstructured": "Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648.",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.8630",
"author": "ES Rosenberg",
"doi-asserted-by": "publisher",
"first-page": "2493",
"issue": "24",
"journal-title": "JAMA",
"key": "177_CR39",
"unstructured": "Rosenberg ES, Dufort EM, Udo T, Wilberschied LA, Kumar J, Tesoriero J, Weinberg P, Kirkwood J, Muse A, DeHovitz J, et al. Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA. 2020;323(24):2493–502. https://doi.org/10.1001/jama.2020.8630.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26165",
"author": "L Kolilekas",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol.",
"key": "177_CR40",
"unstructured": "Kolilekas L, Loverdos K, Giannakaki S, Vlassi L, Levounets A, Zervas E, Gaga M. Can steroids reverse the severe COVID-19 induced ‘cytokine storm’? J Med Virol. 2020. https://doi.org/10.1002/jmv.26165.",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa601",
"author": "R Fadel",
"doi-asserted-by": "publisher",
"journal-title": "Clin Infect Dis.",
"key": "177_CR41",
"unstructured": "Fadel R, Morrison AR, Vahia A, Smith ZR, Chaudhry Z, Bhargava P, Miller J, Kenney RM, Alangaden G, Ramesh MS. Henry Ford COVID-19 Management Task Force Early short course corticosteroids in hospitalized patients with COVID-19. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa601.",
"year": "2020"
},
{
"DOI": "10.1002/rcr2.596",
"author": "C So",
"doi-asserted-by": "crossref",
"first-page": "e00596",
"issue": "6",
"journal-title": "Respirol Case Rep.",
"key": "177_CR42",
"unstructured": "So C, Ro S, Murakami M, Imai R, Jinta T. High-dose, short-term corticosteroids for ARDS caused by COVID-19: a case series. Respirol Case Rep. 2020;8(6):e00596.",
"volume": "8",
"year": "2020"
},
{
"author": "C Wu",
"first-page": "1",
"issue": "7",
"journal-title": "China. JAMA Intern Med.",
"key": "177_CR43",
"unstructured": "Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China. JAMA Intern Med. 2020;180(7):1–11.",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1097/SHK.0000000000001574",
"author": "M Yuan",
"doi-asserted-by": "publisher",
"journal-title": "Shock.",
"key": "177_CR44",
"unstructured": "Yuan M, Xu X, Xia D, Tao Z, Yin W, Tan W, Hu Y, Song C. Effects of corticosteroid treatment for non-severe COVID-19 pneumonia: a propensity score-based analysis. Shock. 2020. https://doi.org/10.1097/SHK.0000000000001574.",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.062",
"author": "Z Yang",
"doi-asserted-by": "publisher",
"first-page": "e13",
"issue": "1",
"journal-title": "J Infect",
"key": "177_CR45",
"unstructured": "Yang Z, Liu J, Zhou Y, Zhao X, Zhao Q, Liu J. The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis. J Infect. 2020;81(1):e13–20.",
"volume": "81",
"year": "2020"
},
{
"key": "177_CR46",
"unstructured": "Randomised Evaluation of COVID-19 Therapy (RECOVERY). Low-cost dexamethasone reduces death by up to one third in hospitalised patients with severe respiratory complications of COVID-19. 2020. Available at: https://www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed June 23, 2020."
},
{
"key": "177_CR47",
"unstructured": "Actualización nº 130. Enfermedad por el coronavirus (COVID-19). 08.06.2020. https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/Actualizacion_130_COVID-19.pdf."
}
],
"reference-count": 47,
"references-count": 47,
"relation": {},
"resource": {
"primary": {
"URL": "https://ehoonline.biomedcentral.com/articles/10.1186/s40164-020-00177-z"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cancer Research",
"Oncology",
"Hematology"
],
"subtitle": [],
"title": "Risk factors and outcome of COVID-19 in patients with hematological malignancies",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "9"
}