Utilizing machine learning for survival analysis to identify risk factors for COVID-19 intensive care unit admission: A retrospective cohort study from the United Arab Emirates
Aamna Alshehhi, Taleb M Almansoori, Ahmed R Alsuwaidi, Hiba Alblooshi
PLOS ONE, doi:10.1371/journal.pone.0291373
Background The current situation of the unprecedented COVID-19 pandemic leverages Artificial Intelligence (AI) as an innovative tool for addressing the evolving clinical challenges. An example is utilizing Machine Learning (ML) models-a subfield of AI that take advantage of observational data/Electronic Health Records (EHRs) to support clinical decision-making for COVID-19 cases. This study aimed to evaluate the clinical characteristics and risk factors for COVID-19 patients in the United Arab Emirates utilizing EHRs and ML for survival analysis models.
Methods We tested various ML models for survival analysis in this work we trained those models using a different subset of features extracted by several feature selection methods. Finally, the best model was evaluated and interpreted using goodness-of-fit based on calibration curves,Partial Dependence Plots and concordance index.
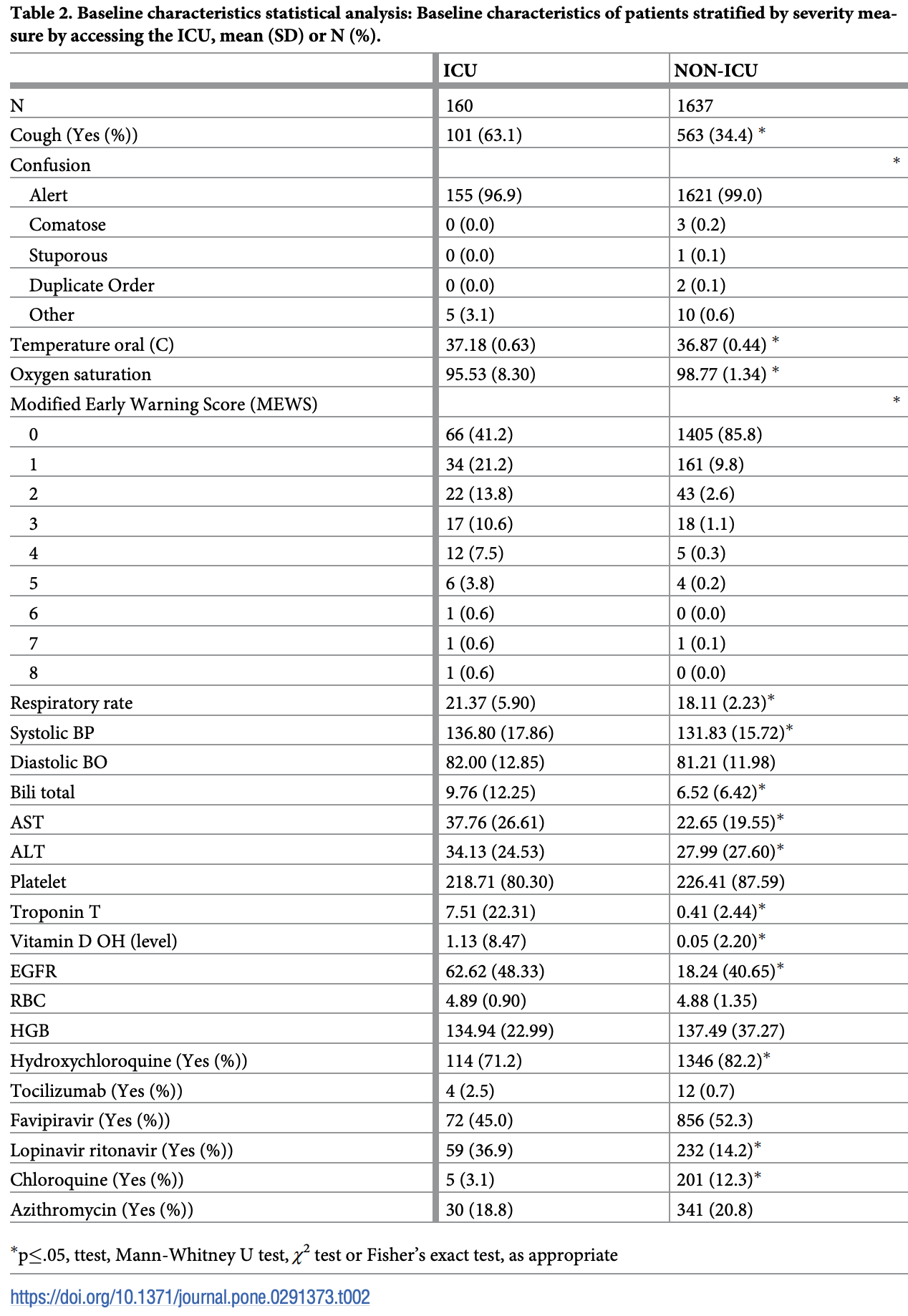
Results The risk of severe disease increases with elevated levels of C-reactive protein, ferritin, lactate dehydrogenase, Modified Early Warning Score, respiratory rate and troponin. The risk also increases with hypokalemia, oxygen desaturation and lower estimated glomerular filtration rate and hypocalcemia and lymphopenia.
Supporting information S1
Author Contributions Conceptualization: Aamna AlShehhi, Taleb M. Almansoori, Ahmed R. Alsuwaidi, Hiba Alblooshi. Data curation: Hiba Alblooshi. Formal analysis: Aamna AlShehhi. Investigation: Taleb M. Almansoori, Ahmed R. Alsuwaidi, Hiba Alblooshi. Methodology: Aamna AlShehhi. Project administration: Hiba Alblooshi. Resources: Taleb M. Almansoori, Ahmed R. Alsuwaidi. Validation: Taleb M. Almansoori, Ahmed R. Alsuwaidi. Visualization: Aamna AlShehhi. Writing -original draft: Aamna AlShehhi, Hiba Alblooshi. Writing -review & editing: Taleb M. Almansoori, Ahmed R. Alsuwaidi, Hiba Alblooshi.
References
Alemzadeh, Alemzadeh, Ziaee, Abedi, Salehiniya, The effect of low serum calcium level on the severity and mortality of Covid patients: A systematic review and meta-analysis, Immunity, Inflammation And Disease,
doi:10.1002/iid3.528Alfano, Ferrari, Fontana, Perrone, Mori et al., The Modena Covid-19 Working Group (MoCo19) Hypokalemia in Patients with COVID-19, Clinical And Experimental Nephrology,
doi:10.1007/s10157-020-01996-4Austin, Harrell, Klaveren, Graphical calibration curves and the integrated calibration index (ICI) for survival models, Statistics In Medicine,
doi:10.1002/sim.8570Carubbi, Salvati, Alunno, Maggi, Borghi et al., Ferritin is associated with the severity of lung involvement but not with worse prognosis in patients with COVID-19: data from two Italian COVID-19 units, Scientific Reports,
doi:10.1038/s41598-021-83831-8Chang, Deng, Jiang, Long, Multiple imputation for analysis of incomplete data in distributed health data networks, Nature Communications,
doi:10.1038/s41467-020-19270-2Chen, Li, Song, Hu, Su et al., Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China, JAMA Network Open,
doi:10.1001/jamanetworkopen.2020.11122Dyusupova, Faizova, Yurkovskaya, Belyaeva, Terekhova et al., Clinical characteristics and risk factors for disease severity and mortality of COVID-19 patients with diabetes mellitus in Kazakhstan: A nationwide study, Heliyon
Ghizlane, Manal, Abderrahim, Abdelilah, Mohammed et al., Lymphopenia in Covid-19: A single center retrospective study of 589 cases, Annals Of Medicine And Surgery,
doi:10.1016/j.amsu.2021.102816Guadiana-Romualdo, Morell-Garcı ´a, Rodrı ´guez-Fraga, Morales-Indiano, Marı et al., Cardiac troponin and COVID-19 severity: Results from BIOCOVID study, European Journal Of Clinical Investigation,
doi:10.1111/eci.13532Hassanipour, Arab-Zozani, Amani, Heidarzad, Fathalipour et al., The efficacy and safety of Favipiravir in treatment of COVID-19: a systematic review and meta-analysis of clinical trials, Scientific Reports,
doi:10.1038/s41598-021-90551-6Hennekens, Rane, Solano, Alter, Johnson et al., Updates on Hydroxychloroquine in Prevention and Treatment of COVID-19, The American Journal Of Medicine,
doi:10.1016/j.amjmed.2021.07.035Henry, Aggarwal, Wong, Benoit, Vikse et al., Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis, The American Journal Of Emergency Medicine
Holman, Knighton, Kar, O'keefe, Curley et al., Risk factors for COVID-19related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, The Lancet Diabetes & Endocrinology,
doi:10.1016/S2213-8587(20)30271-0Huang, Pranata, Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis, Journal Of Intensive Care,
doi:10.1186/s40560-020-00453-4Li, Wang, Liu, Wang, Lin et al., Exploration of prognostic factors for critical COVID-19 patients using a nomogram model, Scientific Reports,
doi:10.1038/s41598-021-87373-xLi, Yan, Chaudhary, Avula, Mudiganti et al., Imputation of missing values for electronic health record laboratory data, Npj Digital Medicine,
doi:10.1038/s41746-021-00518-0Lin, Yan, Chen, Wu, Liu et al., Role of a lower cutoff of high sensitivity troponin I in identification of early cardiac damage in non-severe patients with COVID-19, Scientific Reports,
doi:10.1038/s41598-022-06378-2Manabe, Kambayashi, Akatsu, Kudo, Favipiravir for the treatment of patients with COVID-19: a systematic review and meta-analysis, BMC Infectious Diseases,
doi:10.1186/s12879-021-06164-xManocha, Kirzner, Ying, Yeo, Peltzer et al., Troponin and Other Biomarker Levels and Outcomes Among Patients Hospitalized With COVID-19: Derivation and Validation of the HA(2)T (2) COVID-19 Mortality Risk Score, Journal Of The American Heart Association,
doi:10.1161/JAHA.120.018477Mcgurnaghan, Weir, Bishop, Kennedy, Blackbourn et al., Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland, The Lancet Diabetes & Endocrinology,
doi:10.1016/S2213-8587(20)30405-8Moncada-Torres, Maaren, Hendriks, Siesling, Geleijnse, Explainable machine learning can outperform Cox regression predictions and provide insights in breast cancer survival, Scientific Reports,
doi:10.1038/s41598-021-86327-7Moreno-Pe ´rez, Leon-Ramirez, Fuertes-Kenneally, Perdiguero, Andres et al., Hypokalemia as a sensitive biomarker of disease severity and the requirement for invasive mechanical ventilation requirement in COVID-19 pneumonia: A case series of 306 Mediterranean patients, International Journal Of Infectious Diseases,
doi:10.1016/j.ijid.2020.09.033Nemati, Ansary, Nemati, Machine-Learning Approaches in COVID-19 Survival Analysis and Discharge-Time Likelihood Prediction Using Clinical Data, Patterns
Papamanoli, Kalogeropoulos, Hotelling, Yoo, Grewal et al., Association of Serum Ferritin Levels and Methylprednisolone Treatment With Outcomes in Nonintubated Patients With Severe COVID-19 Pneumonia, JAMA Network Open,
doi:10.1001/jamanetworkopen.2021.27172Petrilli, Jones, Yang, Rajagopalan, O'donnell et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Reis, Silva, Silva, Thabane, Singh et al., TOGETHER Investigators Effect of Early Treatment With Hydroxychloroquine or Lopinavir and Ritonavir on Risk of Hospitalization Among Patients With COVID-19: The TOGETHER Randomized Clinical Trial, JAMA Network Open,
doi:10.1001/jamanetworkopen.2021.6468Schwab, Mehrjou, Parbhoo, Celi, Hetzel et al., Real-time prediction of COVID-19 related mortality using electronic health records, Nature Communications,
doi:10.1038/s41467-020-20816-7Shih, Johnson, Maki, Hennekens, Hydroxychloroquine for Coronavirus: The Urgent Need for a Moratorium on Prescriptions, The American Journal Of Medicine,
doi:10.1016/j.amjmed.2020.05.005Sim, Chidambaram, Wong, Pathmanathan, Peariasamy et al., Clinical characteristics and risk factors for severe COVID-19 infections in Malaysia: A nationwide observational study, The Lancet Regional Health Western Pacific,
doi:10.1016/j.lanwpc.2020.100055Soltan, Kouchaki, Zhu, Kiyasseh, Taylor et al., Rapid triage for COVID-19 using routine clinical data for patients attending hospital: development and prospective validation of an artificial intelligence screening test, The Lancet Digital Health,
doi:10.1016/S2589-7500(20)30274-0Spooner, Chen, Sowmya, Sachdev, Kochan et al., A comparison of machine learning methods for survival analysis of high-dimensional clinical data for dementia prediction, Scientific Reports,
doi:10.1038/s41598-020-77220-wSteele, Denaxas, Shah, Hemingway, Luscombe, Machine learning models in electronic health records can outperform conventional survival models for predicting patient mortality in coronary artery disease, PLOS ONE,
doi:10.1371/journal.pone.0202344Tan, Wang, Zhang, Ding, Huang et al., Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study, Signal Transduction And Targeted Therapy,
doi:10.1038/s41392-020-0148-4Thomson, Nachlis, Emergency Use Authorizations During the COVID-19 Pandemic: Lessons From Hydroxychloroquine for Vaccine Authorization and Approval, JAMA,
doi:10.1001/jama.2020.16253Tobin, Laghi, Jubran, Why COVID-19 Silent Hypoxemia is Baffling to Physicians, American Journal Of Respiratory And Critical Care Medicine,
doi:10.1164/rccm.202006-2157CPTorres, Alcubilla, Gonza ´lez-Cordo ´n, Inciarte, Chumbita et al., COVID19 Hospital Clı ´nic Infectious Diseases Research Group Impact of low serum calcium at hospital admission on SARS-CoV-2 infection outcome, International Journal Of Infectious Diseases: IJID: Official Publication Of The International Society For Infectious Diseases,
doi:10.1016/j.ijid.2020.11.207Uribarri, Nu ´ñez-Gil, Aparisi, Becerra-Muñoz, Feltes et al., Impact of renal function on admission in COVID-19 patients: an analysis of the international HOPE COVID-19 (Health Outcome Predictive Evaluation for COVID 19) Registry, Journal Of Nephrology,
doi:10.1007/s40620-020-00790-5Wang, Li, Reddy, Machine Learning for Survival Analysis: A Survey, ACM Comput. Surv
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature,
doi:10.1038/s41586-020-2521-4Xia, Zhang, Xu, Wang, Yuan et al., Early kidney injury predicts disease progression in patients with COVID-19: a cohort study, BMC Infectious Diseases,
doi:10.1186/s12879-021-06576-9Xiang, Fei, Xiang, Xu, Zheng et al., Renal dysfunction and prognosis of COVID-19 patients: a hospital-based retrospective cohort study, BMC Infectious Diseases,
doi:10.1186/s12879-021-05861-xXie, Covassin, Fan, Singh, Gao et al., Association Between Hypoxemia and Mortality in Patients With COVID-19, Mayo Clinic Proceedings,
doi:10.1016/j.mayocp.2020.04.006Yitbarek, Ayehu, Asnakew, Ayele, Bariso Gare et al., The role of C-reactive protein in predicting the severity of COVID-19 disease: A systematic review, SAGE Open Medicine,
doi:10.1177/20503121211050755DOI record:
{
"DOI": "10.1371/journal.pone.0291373",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0291373",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Background</jats:title>\n<jats:p>The current situation of the unprecedented COVID-19 pandemic leverages Artificial Intelligence (AI) as an innovative tool for addressing the evolving clinical challenges. An example is utilizing Machine Learning (ML) models—a subfield of AI that take advantage of observational data/Electronic Health Records (EHRs) to support clinical decision-making for COVID-19 cases. This study aimed to evaluate the clinical characteristics and risk factors for COVID-19 patients in the United Arab Emirates utilizing EHRs and ML for survival analysis models.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>We tested various ML models for survival analysis in this work we trained those models using a different subset of features extracted by several feature selection methods. Finally, the best model was evaluated and interpreted using goodness-of-fit based on calibration curves,Partial Dependence Plots and concordance index.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Results</jats:title>\n<jats:p>The risk of severe disease increases with elevated levels of C-reactive protein, ferritin, lactate dehydrogenase, Modified Early Warning Score, respiratory rate and troponin. The risk also increases with hypokalemia, oxygen desaturation and lower estimated glomerular filtration rate and hypocalcemia and lymphopenia.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusion</jats:title>\n<jats:p>Analyzing clinical data using AI models can provide vital information for clinician to measure the risk of morbidity and mortality of COVID-19 patients. Further validation is crucial to implement the model in real clinical settings.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1868-1003",
"affiliation": [],
"authenticated-orcid": true,
"family": "AlShehhi",
"given": "Aamna",
"sequence": "first"
},
{
"affiliation": [],
"family": "Almansoori",
"given": "Taleb M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alsuwaidi",
"given": "Ahmed R.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9229-8726",
"affiliation": [],
"authenticated-orcid": true,
"family": "Alblooshi",
"given": "Hiba",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2024,
1,
11
]
],
"date-time": "2024-01-11T18:23:56Z",
"timestamp": 1704997436000
},
"deposited": {
"date-parts": [
[
2024,
1,
11
]
],
"date-time": "2024-01-11T18:24:37Z",
"timestamp": 1704997477000
},
"editor": [
{
"affiliation": [],
"family": "Reyes",
"given": "Luis Felipe",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2024,
1,
12
]
],
"date-time": "2024-01-12T00:23:24Z",
"timestamp": 1705019004106
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
1,
11
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
1,
11
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
11
]
],
"date-time": "2024-01-11T00:00:00Z",
"timestamp": 1704931200000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0291373",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0291373",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2024,
1,
11
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
11
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.1016/j.heliyon.2021.e06561",
"article-title": "Clinical characteristics and risk factors for disease severity and mortality of COVID-19 patients with diabetes mellitus in Kazakhstan: A nationwide study",
"author": "A. Dyusupova",
"doi-asserted-by": "crossref",
"first-page": "e06561",
"issue": "3",
"journal-title": "Heliyon",
"key": "pone.0291373.ref001",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/j.patter.2020.100074",
"article-title": "Machine-Learning Approaches in COVID-19 Survival Analysis and Discharge-Time Likelihood Prediction Using Clinical Data",
"author": "M. Nemati",
"doi-asserted-by": "crossref",
"first-page": "100074",
"issue": "8",
"journal-title": "Patterns",
"key": "pone.0291373.ref002",
"volume": "1",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "E. Williamson",
"doi-asserted-by": "crossref",
"first-page": "430",
"issue": "8",
"journal-title": "Nature",
"key": "pone.0291373.ref003",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-20816-7",
"article-title": "Real-time prediction of COVID-19 related mortality using electronic health records",
"author": "P. Schwab",
"doi-asserted-by": "crossref",
"first-page": "1058",
"issue": "2",
"journal-title": "Nature Communications",
"key": "pone.0291373.ref004",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/S2589-7500(20)30274-0",
"article-title": "Rapid triage for COVID-19 using routine clinical data for patients attending hospital: development and prospective validation of an artificial intelligence screening test",
"author": "A. Soltan",
"doi-asserted-by": "crossref",
"first-page": "e78",
"issue": "2",
"journal-title": "The Lancet Digital Health",
"key": "pone.0291373.ref005",
"volume": "3",
"year": "2021"
},
{
"article-title": "Clinical characteristics and risk factors for severe COVID-19 infections in Malaysia: A nationwide observational study",
"author": "B. Sim",
"issue": "11",
"journal-title": "The Lancet Regional Health Western Pacific",
"key": "pone.0291373.ref006",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "N. Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"issue": "10",
"journal-title": "The Lancet Diabetes & Endocrinology",
"key": "pone.0291373.ref007",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30405-8",
"article-title": "Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland",
"author": "S. McGurnaghan",
"doi-asserted-by": "crossref",
"first-page": "82",
"issue": "2",
"journal-title": "The Lancet Diabetes & Endocrinology",
"key": "pone.0291373.ref008",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1136/bmj.m1966",
"article-title": "Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study",
"author": "C. Petrilli",
"doi-asserted-by": "crossref",
"first-page": "m1966",
"issue": "5",
"journal-title": "BMJ",
"key": "pone.0291373.ref009",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1038/s41598-020-77220-w",
"article-title": "A comparison of machine learning methods for survival analysis of high-dimensional clinical data for dementia prediction",
"author": "A. Spooner",
"doi-asserted-by": "crossref",
"first-page": "20410",
"issue": "11",
"journal-title": "Scientific Reports",
"key": "pone.0291373.ref010",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-19270-2",
"article-title": "Multiple imputation for analysis of incomplete data in distributed health data networks",
"author": "C. Chang",
"doi-asserted-by": "crossref",
"first-page": "5467",
"issue": "10",
"journal-title": "Nature Communications",
"key": "pone.0291373.ref011",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/s41746-021-00518-0",
"article-title": "Imputation of missing values for electronic health record laboratory data",
"author": "J. Li",
"doi-asserted-by": "crossref",
"first-page": "147",
"issue": "10",
"journal-title": "Npj Digital Medicine",
"key": "pone.0291373.ref012",
"volume": "4",
"year": "2021"
},
{
"article-title": "Machine Learning for Survival Analysis: A Survey",
"author": "P. Wang",
"issue": "2",
"journal-title": "ACM Comput. Surv",
"key": "pone.0291373.ref013",
"volume": "51",
"year": "2019"
},
{
"DOI": "10.1038/s41598-021-86327-7",
"article-title": "Explainable machine learning can outperform Cox regression predictions and provide insights in breast cancer survival",
"author": "A. Moncada-Torres",
"doi-asserted-by": "crossref",
"first-page": "6968",
"issue": "3",
"journal-title": "Scientific Reports",
"key": "pone.0291373.ref014",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0202344",
"article-title": "Machine learning models in electronic health records can outperform conventional survival models for predicting patient mortality in coronary artery disease",
"author": "A. Steele",
"doi-asserted-by": "crossref",
"first-page": "e0202344",
"issue": "8",
"journal-title": "PLOS ONE",
"key": "pone.0291373.ref015",
"volume": "13",
"year": "2018"
},
{
"DOI": "10.1002/sim.8570",
"article-title": "Graphical calibration curves and the integrated calibration index (ICI) for survival models",
"author": "P. Austin",
"doi-asserted-by": "crossref",
"first-page": "2714",
"issue": "9",
"journal-title": "Statistics In Medicine",
"key": "pone.0291373.ref016",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-87373-x",
"article-title": "Exploration of prognostic factors for critical COVID-19 patients using a nomogram model",
"author": "J. Li",
"doi-asserted-by": "crossref",
"first-page": "8192",
"issue": "4",
"journal-title": "Scientific Reports",
"key": "pone.0291373.ref017",
"volume": "11",
"year": "2021"
},
{
"article-title": "The role of C-reactive protein in predicting the severity of COVID-19 disease: A systematic review",
"author": "G. Yitbarek",
"issue": "1",
"journal-title": "SAGE Open Medicine",
"key": "pone.0291373.ref018",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.ajem.2020.05.073",
"article-title": "Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis",
"author": "B. Henry",
"doi-asserted-by": "crossref",
"first-page": "1722",
"issue": "9",
"journal-title": "The American Journal Of Emergency Medicine",
"key": "pone.0291373.ref019",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-83831-8",
"article-title": "Ferritin is associated with the severity of lung involvement but not with worse prognosis in patients with COVID-19: data from two Italian COVID-19 units",
"author": "F. Carubbi",
"doi-asserted-by": "crossref",
"first-page": "4863",
"issue": "3",
"journal-title": "Scientific Reports",
"key": "pone.0291373.ref020",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.27172",
"article-title": "Association of Serum Ferritin Levels and Methylprednisolone Treatment With Outcomes in Nonintubated Patients With Severe COVID-19 Pneumonia",
"author": "A. Papamanoli",
"doi-asserted-by": "crossref",
"first-page": "e2127172",
"issue": "10",
"journal-title": "JAMA Network Open",
"key": "pone.0291373.ref021",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1002/iid3.528",
"article-title": "The effect of low serum calcium level on the severity and mortality of Covid patients: A systematic review and meta-analysis",
"author": "E. Alemzadeh",
"doi-asserted-by": "crossref",
"first-page": "1219",
"journal-title": "Immunity, Inflammation And Disease",
"key": "pone.0291373.ref022",
"volume": "9",
"year": "2021"
},
{
"article-title": "Impact of low serum calcium at hospital admission on SARS-CoV-2 infection outcome",
"author": "COVID19 Hospital Clínic Infectious Diseases Research Group",
"first-page": "164",
"issue": "3",
"journal-title": "International Journal Of Infectious Diseases: IJID: Official Publication Of The International Society For Infectious Diseases",
"key": "pone.0291373.ref023",
"volume": "104",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.11122",
"article-title": "Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China",
"author": "D. Chen",
"doi-asserted-by": "crossref",
"first-page": "e2011122",
"issue": "6",
"journal-title": "JAMA Network Open",
"key": "pone.0291373.ref024",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.09.033",
"article-title": "Hypokalemia as a sensitive biomarker of disease severity and the requirement for invasive mechanical ventilation requirement in COVID-19 pneumonia: A case series of 306 Mediterranean patients",
"author": "O. Moreno-Pérez",
"doi-asserted-by": "crossref",
"first-page": "449",
"issue": "11",
"journal-title": "International Journal Of Infectious Diseases",
"key": "pone.0291373.ref025",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1007/s10157-020-01996-4",
"article-title": "Hypokalemia in Patients with COVID-19",
"author": "The Modena Covid-19 Working Group (MoCo19)",
"doi-asserted-by": "crossref",
"first-page": "401",
"issue": "4",
"journal-title": "Clinical And Experimental Nephrology",
"key": "pone.0291373.ref026",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1038/s41392-020-0148-4",
"article-title": "Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study",
"author": "L. Tan",
"doi-asserted-by": "crossref",
"first-page": "33",
"issue": "3",
"journal-title": "Signal Transduction And Targeted Therapy",
"key": "pone.0291373.ref027",
"volume": "5",
"year": "2020"
},
{
"article-title": "Lymphopenia in Covid-19: A single center retrospective study of 589 cases",
"author": "E. Ghizlane",
"first-page": "102816",
"issue": "9",
"journal-title": "Annals Of Medicine And Surgery (2012)",
"key": "pone.0291373.ref028",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.1186/s40560-020-00453-4",
"article-title": "Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis",
"author": "I. Huang",
"doi-asserted-by": "crossref",
"first-page": "36",
"issue": "5",
"journal-title": "Journal Of Intensive Care",
"key": "pone.0291373.ref029",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.mayocp.2020.04.006",
"article-title": "Association Between Hypoxemia and Mortality in Patients With COVID-19",
"author": "J. Xie",
"doi-asserted-by": "crossref",
"first-page": "1138",
"issue": "6",
"journal-title": "Mayo Clinic Proceedings",
"key": "pone.0291373.ref030",
"volume": "95",
"year": "2020"
},
{
"article-title": "Why COVID-19 Silent Hypoxemia is Baffling to Physicians",
"author": "M. Tobin",
"issue": "6",
"journal-title": "American Journal Of Respiratory And Critical Care Medicine",
"key": "pone.0291373.ref031",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.1038/s41598-022-06378-2",
"article-title": "Role of a lower cutoff of high sensitivity troponin I in identification of early cardiac damage in non-severe patients with COVID-19",
"author": "Y. Lin",
"doi-asserted-by": "crossref",
"first-page": "2389",
"issue": "2",
"journal-title": "Scientific Reports",
"key": "pone.0291373.ref032",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1161/JAHA.120.018477",
"article-title": "Troponin and Other Biomarker Levels and Outcomes Among Patients Hospitalized With COVID-19: Derivation and Validation of the HA(2)T(2) COVID-19 Mortality Risk Score",
"author": "K. Manocha",
"doi-asserted-by": "crossref",
"first-page": "e018477",
"issue": "3",
"journal-title": "Journal Of The American Heart Association",
"key": "pone.0291373.ref033",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1111/eci.13532",
"article-title": "Cardiac troponin and COVID-19 severity: Results from BIOCOVID study",
"author": "L. Guadiana-Romualdo",
"doi-asserted-by": "crossref",
"first-page": "e13532",
"issue": "6",
"journal-title": "European Journal Of Clinical Investigation",
"key": "pone.0291373.ref034",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-05861-x",
"article-title": "Renal dysfunction and prognosis of COVID-19 patients: a hospital-based retrospective cohort study",
"author": "H. Xiang",
"doi-asserted-by": "crossref",
"first-page": "158",
"issue": "2",
"journal-title": "BMC Infectious Diseases",
"key": "pone.0291373.ref035",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1007/s40620-020-00790-5",
"article-title": "Impact of renal function on admission in COVID-19 patients: an analysis of the international HOPE COVID-19 (Health Outcome Predictive Evaluation for COVID 19) Registry",
"author": "A. Uribarri",
"doi-asserted-by": "crossref",
"first-page": "737",
"issue": "8",
"journal-title": "Journal Of Nephrology",
"key": "pone.0291373.ref036",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1186/s12879-021-06576-9",
"article-title": "Early kidney injury predicts disease progression in patients with COVID-19: a cohort study",
"author": "T. Xia",
"doi-asserted-by": "crossref",
"first-page": "1012",
"issue": "9",
"journal-title": "BMC Infectious Diseases",
"key": "pone.0291373.ref037",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.6468",
"article-title": "Effect of Early Treatment With Hydroxychloroquine or Lopinavir and Ritonavir on Risk of Hospitalization Among Patients With COVID-19: The TOGETHER Randomized Clinical Trial",
"author": "TOGETHER Investigators",
"doi-asserted-by": "crossref",
"first-page": "e216468",
"issue": "4",
"journal-title": "JAMA Network Open",
"key": "pone.0291373.ref038",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.amjmed.2020.05.005",
"article-title": "Hydroxychloroquine for Coronavirus: The Urgent Need for a Moratorium on Prescriptions",
"author": "R. Shih",
"doi-asserted-by": "crossref",
"first-page": "1007",
"issue": "9",
"journal-title": "The American Journal Of Medicine",
"key": "pone.0291373.ref039",
"volume": "133",
"year": "2020"
},
{
"DOI": "10.1016/j.amjmed.2021.07.035",
"article-title": "Updates on Hydroxychloroquine in Prevention and Treatment of COVID-19",
"author": "C. Hennekens",
"doi-asserted-by": "crossref",
"first-page": "7",
"issue": "1",
"journal-title": "The American Journal Of Medicine",
"key": "pone.0291373.ref040",
"volume": "135",
"year": "2022"
},
{
"DOI": "10.1001/jama.2020.16253",
"article-title": "Emergency Use Authorizations During the COVID-19 Pandemic: Lessons From Hydroxychloroquine for Vaccine Authorization and Approval",
"author": "K. Thomson",
"doi-asserted-by": "crossref",
"first-page": "1282",
"issue": "10",
"journal-title": "JAMA",
"key": "pone.0291373.ref041",
"volume": "324",
"year": "2020"
},
{
"key": "pone.0291373.ref042",
"unstructured": "Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine, https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chloroquine-and, 14 04 2022."
},
{
"DOI": "10.1038/s41598-021-90551-6",
"article-title": "The efficacy and safety of Favipiravir in treatment of COVID-19: a systematic review and meta-analysis of clinical trials",
"author": "S. Hassanipour",
"doi-asserted-by": "crossref",
"first-page": "11022",
"issue": "5",
"journal-title": "Scientific Reports",
"key": "pone.0291373.ref043",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-06164-x",
"article-title": "Favipiravir for the treatment of patients with COVID-19: a systematic review and meta-analysis",
"author": "T. Manabe",
"doi-asserted-by": "crossref",
"first-page": "489",
"issue": "5",
"journal-title": "BMC Infectious Diseases",
"key": "pone.0291373.ref044",
"volume": "21",
"year": "2021"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0291373"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Utilizing machine learning for survival analysis to identify risk factors for COVID-19 intensive care unit admission: A retrospective cohort study from the United Arab Emirates",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "19"
}