The Association between Acute Cardiac Injury and Outcomes of Hospitalized Patients with COVID-19: Long-Term Follow-up Results from the Sina Hospital COVID-19 Registry, Iran
MD Danesh Soltani, MD Azar Hadadi, MD Shahrokh Karbalai Saleh, MD Alireza Oraii, MD Azadeh Sadatnaseri, MD Mostafa Roozitalab, MD Zahra Shajari, MD Shima Sadat Ghaemmaghami, MD Haleh Ashraf
Background: The present study aimed to investigate the association between acute cardiac injury (ACI) and outcomes in hospitalized patients with coronavirus disease 2019 (COVID-19) in Iran.
Methods: The current cohort study enrolled all consecutive hospitalized patients with COVID-19 (≥ 18 y) who had serum high-sensitivity cardiac troponin-I (hs-cTnT) measurements on admission between March 2020 and March 2021. ACI was determined as hs-cTnT levels exceeding the 99th percentile of normal values. Data on demographics, comorbidities, clinical and laboratory characteristics, and outcomes were collected from Web-based electronic health records.
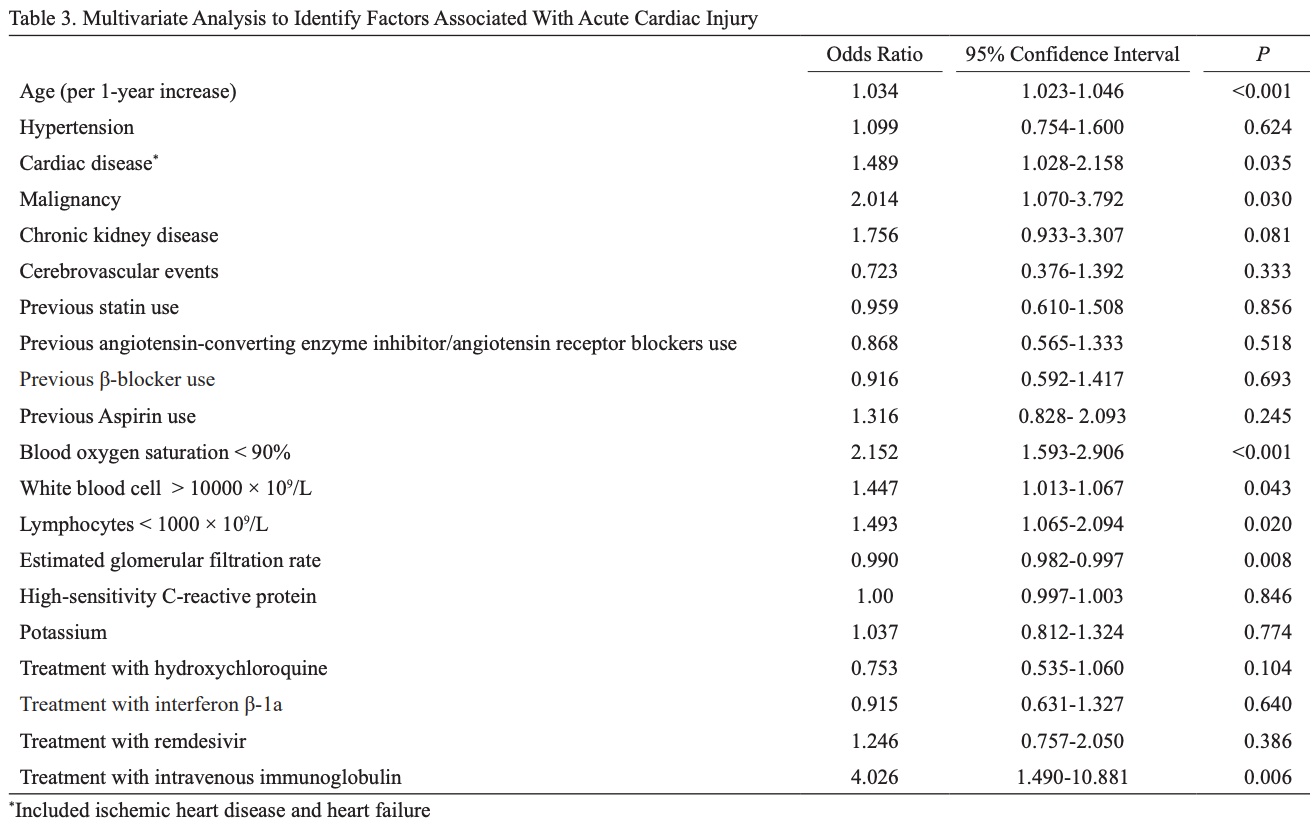
Results: The study population consisted of 1413 hospitalized patients with COVID-19, of whom 319 patients (22.58%) presented with ACI. The patients with ACI had a significantly higher mortality rate than those without ACI (48.28% vs 15.63%; P<0.001) within a mean follow-up of 218.86 days from symptom onset. ACI on admission was independently associated with mortality (HR, 1.44; P=0.018). In multivariable logistic regression, age (OR, 1.034; P<0.001), preexisting cardiac disease (OR, 1.49; P=0.035), preexisting malignancy (OR, 2.01; P=0.030), oxygen saturation reduced to less than 90% (OR, 2.15; P<0.001), leukocytosis (OR, 1.45; P=0.043), lymphopenia (OR, 1.49; P=0.020), reduced estimated glomerular filtration rates (eGFRs) (OR, 0.99; P=0.008), and treatment with intravenous immunoglobulin during hospitalization (OR, 4.03; P=0.006) were independently associated with ACI development. Conclusion: ACI occurrence on admission was associated with long-term mortality in our hospitalized patients with COVID-19. The finding further underscores the significance of evaluating ACI occurrence on admission, particularly in individuals more prone to ACI, including older individuals and those with preexisting comorbidities, reduced oxygen saturation, and increased inflammatory responses.
Supplementary Material
References
Ards Definition, Force, Ranieri, Rubenfeld, Thompson et al., Acute respiratory distress syndrome: the Berlin Definition, JAMA
Bavishi, Bonow, Trivedi, Abbott, Messerli et al., Special Article -Acute myocardial injury in patients hospitalized with COVID-19 infection: A review, Prog Cardiovasc Dis
Bernheim, Mei, Huang, Yang, Fayad et al., Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection, Radiology
Davé, Hagan, Myocardial infarction during intravenous immunoglobulin infusion in a 65-year-old man with common variable immunodeficiency and subsequent successful repeated administration, Ann Allergy Asthma Immunol
Egbuche, Jegede, Abe, Wagle, Huynh et al., Pre-existing cardiovascular disease, acute kidney injury, and cardiovascular outcomes in hospitalized blacks with COVID-19 infection, Am J Cardiovasc Dis
Elkayam, Paran, Milo, Davidovitz, Almoznino-Sarafian et al., Acute myocardial infarction associated with high dose intravenous immunoglobulin infusion for autoimmune disorders. A study of four cases, Ann Rheum Dis
Figliozzi, Masci, Ahmadi, Tondi, Koutli et al., Predictors of adverse prognosis in COVID-19: A systematic review and meta-analysis, Eur J Clin Invest
Guo, Fan, Chen, Wu, Zhang et al., Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19), JAMA Cardiol
Huang, Huang, Du, Kong, Zhang et al., Prevalence and clinical outcomes of cardiac injury in patients with COVID-19: A systematic review and meta-analysis, Nutr Metab Cardiovasc Dis
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Karahan, Katkat, Ozcan, Sahin, Okuyan, Impact of acute myocardial injury on prognosis in patients with COVID-19, Eur Rev Med Pharmacol Sci
Kellum, Van Till, Mulligan, Targeting acute kidney injury in COVID-19, Nephrol Dial Transplant
Knight, Ho, Pius, Buchan, Carson et al., Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score, BMJ
Lala, Johnson, Januzzi, Russak, Paranjpe et al., Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection, J Am Coll Cardiol
Li, Pan, Li, Xing, Yang et al., Cardiac injury associated with severe disease or ICU admission and death in hospitalized patients with COVID-19: a meta-analysis and systematic review, Crit Care
Li, Xu, Huang, Fei, Xie et al., Acute cardiac injury and acute kidney injury associated with severity and mortality in patients with COVID-19, Eur Rev Med Pharmacol Sci
Manocha, Kirzner, Ying, Yeo, Peltzer et al., Troponin and Other Biomarker Levels and Outcomes Among Patients Hospitalized With COVID-19: Derivation and Validation of the HA2T2 COVID-19 Mortality Risk Score, J Am Heart Assoc
Manolis, Manolis, Manolis, COVID-19 and Acute Myocardial Injury and Infarction: Related Mechanisms and Emerging Challenges, J Cardiovasc Pharmacol Ther
Mccarthy, Raber, Chapman, Sandoval, Apple et al., Myocardial Injury in the Era of High-Sensitivity Cardiac Troponin Assays: A Practical Approach for Clinicians, JAMA Cardiol
Musher, Abers, Vf, Acute Infection and Myocardial Infarction, N Engl J Med
Organization, Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected, Interim guidance
Saleh, Oraii, Soleimani, Hadadi, Shajari et al., The association between cardiac injury and outcomes in hospitalized patients with COVID-19, Intern Emerg Med
Salehi, Abedi, Balakrishnan, Gholamrezanezhad, Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients, AJR Am J Roentgenol
Sandoval, Januzzi, Jr, Jaffe, Cardiac Troponin for Assessment of Myocardial Injury in COVID-19: JACC Review Topic of the Week, J Am Coll Cardiol
Shi, Qin, Shen, Cai, Liu et al., Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China, JAMA Cardiol
Sinclair, Zhu, Xu, Ma, Shi et al., A meta-analysis on the role of pre-existing chronic disease in the cardiac complications of SARS-CoV-2 infection, iScience
Soltani, None
Uribarri, Núñez-Gil, Aparisi, Becerra-Muñoz, Feltes et al., Impact of renal function on admission in COVID-19 patients: an analysis of the international HOPE COVID-19 (Health Outcome Predictive Evaluation for COVID 19) Registry, J Nephrol
Wibowo, Pranata, Akbar, Purnomowati, Martha, Prognostic performance of troponin in COVID-19: A diagnostic meta-analysis and meta-regression, Int J Infect Dis
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention, JAMA
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir Med
Zou, Qian, Wang, Zhao, Bai, Cardiac Injury and COVID-19: A Systematic Review and Meta-analysis, CJC Open
DOI record:
{
"DOI": "10.18502/jthc.v18i3.14114",
"ISSN": [
"2008-2371",
"1735-8620"
],
"URL": "http://dx.doi.org/10.18502/jthc.v18i3.14114",
"abstract": "<jats:p>Background: The present study aimed to investigate the association between acute cardiac injury (ACI) and outcomes in hospitalized patients with coronavirus disease 2019 (COVID-19) in Iran.
\nMethods: The current cohort study enrolled all consecutive hospitalized patients with COVID-19 (≥ 18 y) who had serum high-sensitivity cardiac troponin-I (hs-cTnT) measurements on admission between March 2020 and March 2021. ACI was determined as hs-cTnT levels exceeding the 99th percentile of normal values. Data on demographics, comorbidities, clinical and laboratory characteristics, and outcomes were collected from Web-based electronic health records.
\nResults: The study population consisted of 1413 hospitalized patients with COVID-19, of whom 319 patients (22.58%) presented with ACI. The patients with ACI had a significantly higher mortality rate than those without ACI (48.28% vs 15.63%; P<0.001) within a mean follow-up of 218.86 days from symptom onset. ACI on admission was independently associated with mortality (HR, 1.44; P=0.018). In multivariable logistic regression, age (OR, 1.034; P<0.001), preexisting cardiac disease (OR, 1.49; P=0.035), preexisting malignancy (OR, 2.01; P=0.030), oxygen saturation reduced to less than 90% (OR, 2.15; P<0.001), leukocytosis (OR, 1.45; P=0.043), lymphopenia (OR, 1.49; P=0.020), reduced estimated glomerular filtration rates (eGFRs) (OR, 0.99; P=0.008), and treatment with intravenous immunoglobulin during hospitalization (OR, 4.03; P=0.006) were independently associated with ACI development.
\nConclusion: ACI occurrence on admission was associated with long-term mortality in our hospitalized patients with COVID-19. The finding further underscores the significance of evaluating ACI occurrence on admission, particularly in individuals more prone to ACI, including older individuals and those with preexisting comorbidities, reduced oxygen saturation, and increased inflammatory responses.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Soltani",
"given": "Danesh",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hadadi",
"given": "Azar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saleh",
"given": "Shahrokh Karbalai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Oraii",
"given": "Alireza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sadatnaseri",
"given": "Azadeh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Roozitalab",
"given": "Mostafa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shajari",
"given": "Zahra",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ghaemmaghami",
"given": "Shima Sadat",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ashraf",
"given": "Haleh",
"sequence": "additional"
}
],
"container-title": "The Journal of Tehran University Heart Center",
"container-title-short": "JTHC",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
11,
21
]
],
"date-time": "2023-11-21T12:45:51Z",
"timestamp": 1700570751000
},
"deposited": {
"date-parts": [
[
2024,
1,
1
]
],
"date-time": "2024-01-01T07:25:05Z",
"timestamp": 1704093905000
},
"indexed": {
"date-parts": [
[
2024,
1,
1
]
],
"date-time": "2024-01-01T07:40:40Z",
"timestamp": 1704094840588
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
11,
21
]
]
},
"member": "7770",
"original-title": [],
"prefix": "10.18502",
"published": {
"date-parts": [
[
2023,
11,
21
]
]
},
"published-online": {
"date-parts": [
[
2023,
11,
21
]
]
},
"publisher": "Knowledge E DMCC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://publish.kne-publishing.com/index.php/JTHC/article/view/14114"
},
"secondary": [
{
"URL": "https://jthc.tums.ac.ir/index.php/jthc/article/view/1745"
}
]
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine"
],
"subtitle": [],
"title": "The Association between Acute Cardiac Injury and Outcomes of Hospitalized Patients with COVID-19: Long-term Follow-up Results from the Sina Hospital COVID-19 Registry, Iran",
"type": "journal-article"
}