Clinical signs, symptoms, and severity of COVID-19 in patients with rheumatic diseases during the COVID-19 epidemic
Mansour Salesi, Maryam Sedarat
doi:10.34172/ipp.2023.40568
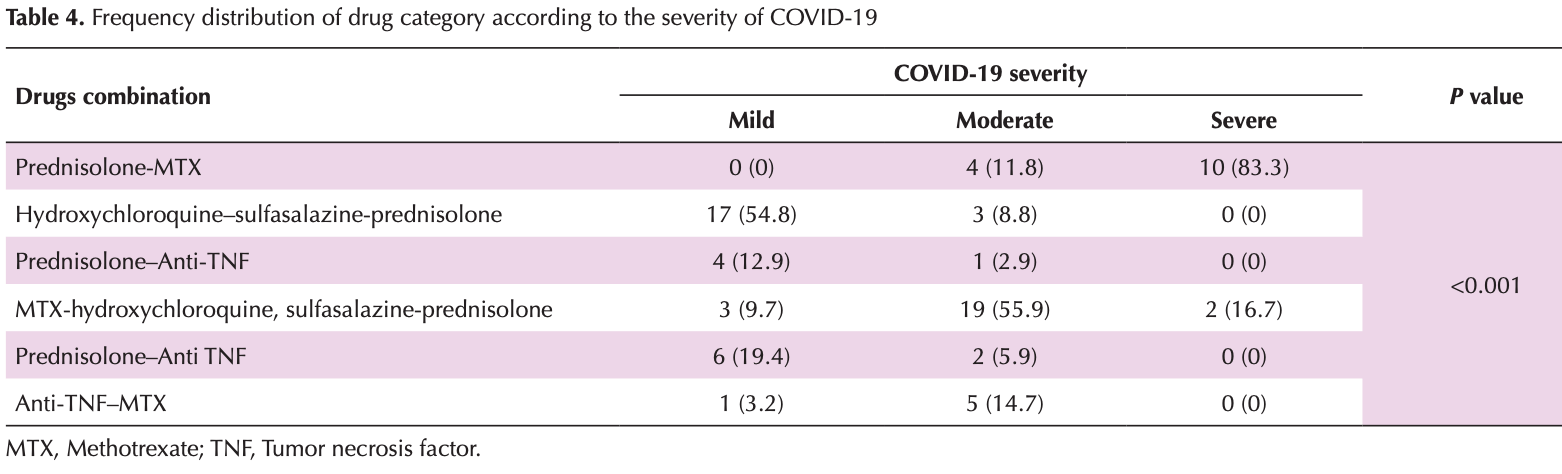
Introduction: Recent studies have shown that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Additionally, certain anti-inflammatory medications have been linked to a reduction in the severity of COVID-19 symptoms. Objectives: This cross-sectional study aimed to determine the frequency of clinical signs, symptoms, and severity of COVID-19 in outpatients with rheumatic diseases. Patients and Methods: A total of 77 patients with rheumatic disorders who were diagnosed with COVID-19 and referred to Isfahan rheumatology clinics in 2020 were selected for this study. The study investigated their clinical signs, symptoms, severity of COVID-19, type of rheumatic disease, and the medications they were using. Furthermore, the study examined the relationship between the severity of COVID-19 and the type of rheumatic disease. Results: Among the 77 patients, 79.2% had rheumatoid arthritis (RA), 9.1% had systemic lupus erythematosus (SLE), 9.1% had Sjogren's syndrome, and 2.6% had other rheumatic disorders. The severity of COVID-19 was classified as mild in 40.3% of cases, moderate in 44.2%, and severe in 15.6%. There was no statistically significant relationship between the type of rheumatic disease and the severity of COVID-19 (P = 0.093).
Conclusion: The findings suggest that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Conversely, the combination of hydroxychloroquine, sulfasalazine, and prednisolone has been associated with a lower prevalence of severe cases of COVID-19. In contrast, the administration of methotrexate and prednisolone has been linked to a higher prevalence of severe cases of COVID-19.
Authors' contribution
Conflicts of interest The authors declare that they have no competing interests.
Ethical issues The research followed the tenets of the Declaration of Helsinki. The Ethics Committee of Isfahan University of Medical Sciences approved this study. The institutional ethical committee at Isfahan University of Medical Sciences approved all study protocols (Ethical code#IR.MUI.MED.REC.1399.883). Accordingly, written informed consent was taken from all participants before any intervention. this study was extracted from a thesis of internal medicine specialty
References
Brownstone, Thibodeaux, Reddy, Myers, Chan et al., Novel Coronavirus Disease (COVID-19) and Biologic Therapy in Psoriasis: Infection Risk and Patient Counseling in Uncertain Times, Dermatol Ther (Heidelb),
doi:10.1007/s13555-020-00377-9Cai, Sun, Huang, Gamber, Wu et al., Indirect virus transmission in a cluster of COVID-19 cases, Wenzhou, China, Emerg Infect Dis,
doi:10.3201/eid2606.200412Chaudhuri, Sasaki, Karkar, Sharif, Lewis et al., Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis, Intensive Care Med,
doi:10.1007/s00134-021-06394-2Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet,
doi:10.1016/S0140-6736(20)30211-7Giacomelli, Pezzati, Conti, Bernacchia, Siano et al., Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study, Clin Infect Dis,
doi:10.1093/cid/ciaa330Jung, Kwon, Choi, Association between previous rheumatoid arthritis and COVID-19 and its severity: a nationwide cohort study in South Korea, BMJ Open,
doi:10.1136/bmjopen-2021-054753Misra, Agarwal, Gasparyan, Zimba, Rheumatologists' perspective on coronavirus disease 19 (COVID-19) and potential therapeutic targets, Clin Rheumatol,
doi:10.1007/s10067-020-05073-9Mukarram, Ghauri, Sethar, Afsar, Riaz et al., COVID-19: an emerging culprit of inflammatory arthritis, Case Rep Rheumatol,
doi:10.1155/2021/6610340Nunez, Leon, Mucientes, Rodriguez-Rodriguez, Urgelles et al., Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases, Ann Rheum Dis,
doi:10.1136/annrheumdis-2020-217984Pan, Ye, Sun, Gui, Liang et al., Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19), Radiology,
doi:10.1148/radiol.2020200370Smolen, Landewé, Bijlsma, Burmester, Chatzidionysiou et al., EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update, Ann Rheum Dis,
doi:10.1136/annrheumdis-2016-210715Spinato, Fabbris, Polesel, Cazzador, Borsetto et al., Alterations in Smell or Taste in Mildly Symptomatic Outpatients With SARS-CoV-2 Infection, JAMA,
doi:10.1001/jama.2020.6771Tong, Wong, Zhu, Fastenberg, Tham, The Prevalence of Olfactory and Gustatory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis, Otolaryngol Head Neck Surg,
doi:10.1177/0194599820926473Tsokos, Lo, Reis, Sullivan, New insights into the immunopathogenesis of systemic lupus erythematosus, Nat Rev Rheumatol,
doi:10.1038/nrrheum.2016.186Wang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA,
doi:10.1001/jama.2020.1585DOI record:
{
"DOI": "10.34172/ipp.2023.40568",
"ISSN": [
"2423-8015"
],
"URL": "http://dx.doi.org/10.34172/ipp.2023.40568",
"abstract": "<jats:p>Introduction: Recent studies have shown that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Additionally, certain anti-inflammatory medications have been linked to a reduction in the severity of COVID-19 symptoms. Objectives: This cross-sectional study aimed to determine the frequency of clinical signs, symptoms, and severity of COVID-19 in outpatients with rheumatic diseases. Patients and Methods: A total of 77 patients with rheumatic disorders who were diagnosed with COVID-19 and referred to Isfahan rheumatology clinics in 2020 were selected for this study. The study investigated their clinical signs, symptoms, severity of COVID-19, type of rheumatic disease, and the medications they were using. Furthermore, the study examined the relationship between the severity of COVID-19 and the type of rheumatic disease. Results: Among the 77 patients, 79.2% had rheumatoid arthritis (RA), 9.1% had systemic lupus erythematosus (SLE), 9.1% had Sjogren’s syndrome, and 2.6% had other rheumatic disorders. The severity of COVID-19 was classified as mild in 40.3% of cases, moderate in 44.2%, and severe in 15.6%. There was no statistically significant relationship between the type of rheumatic disease and the severity of COVID-19 (P=0.093). Conclusion: The findings suggest that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Conversely, the combination of hydroxychloroquine, sulfasalazine, and prednisolone has been associated with a lower prevalence of severe cases of COVID-19. In contrast, the administration of methotrexate and prednisolone has been linked to a higher prevalence of severe cases of COVID-19.</jats:p>",
"assertion": [
{
"label": "Journal Owner",
"name": "journal_owner",
"value": "Nickan Research Institute"
},
{
"label": "Journal Publisher",
"name": "journal_publisher",
"value": "Nickan Research Institute"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "2023-07-16"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2023-10-25"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2023-12-18"
}
],
"author": [
{
"affiliation": [
{
"name": "Acquired Immunodeficiency Research Centre, Isfahan University of Medical Sciences, Isfahan, Iran"
}
],
"family": "Salesi",
"given": "Mansour",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0009-0008-6308-2927",
"affiliation": [
{
"name": "Isfahan University of Medical Sciences, Isfahan, Iran"
}
],
"authenticated-orcid": true,
"family": "Sedarat",
"given": "Maryam",
"sequence": "additional"
}
],
"container-title": "Immunopathologia Persa",
"container-title-short": "Immunopathol Persa",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"immunopathol.com"
]
},
"created": {
"date-parts": [
[
2024,
1,
8
]
],
"date-time": "2024-01-08T11:56:01Z",
"timestamp": 1704714961000
},
"deposited": {
"date-parts": [
[
2024,
1,
8
]
],
"date-time": "2024-01-08T11:56:01Z",
"timestamp": 1704714961000
},
"indexed": {
"date-parts": [
[
2024,
1,
9
]
],
"date-time": "2024-01-09T00:21:40Z",
"timestamp": 1704759700617
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
12,
18
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
1,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://immunopathol.com/PDF/ipp-10-e40568.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://immunopathol.com/PDF/ipp-10-e40568.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "20123",
"original-title": [],
"page": "e40568",
"prefix": "10.34172",
"published": {
"date-parts": [
[
2023,
12,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
12,
18
]
]
},
"publisher": "Maad Rayan Publishing Company",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://immunopathol.com/Article/ipp-40568"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Immunology and Microbiology (miscellaneous)",
"Hematology",
"Immunology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Clinical signs, symptoms, and severity of COVID-19 in patients with rheumatic diseases during the COVID-19 epidemic",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.34172/crossmark_policy",
"volume": "10"
}