The prophylactic effect of hydroxychloroquine on the severity of COVID-19 infection in an asymptomatic population: A randomized clinical trial
Termeh Tarjoman, Mahnaz Valizadeh, Parisa Shojaei, Behnam Farhoo, Mehrangi Zange, Masood Naj, Seyed Hamid Jamaldi, Masoumeh Mesgar, Za Hanifezadeh, Fae Abdollahi, Hamidreza Massumi Naini, Mohsen Alijani, Hasti Ziaee, Dr Arezoo Chouhdari
doi:10.22037/sdh.v10i1.43032
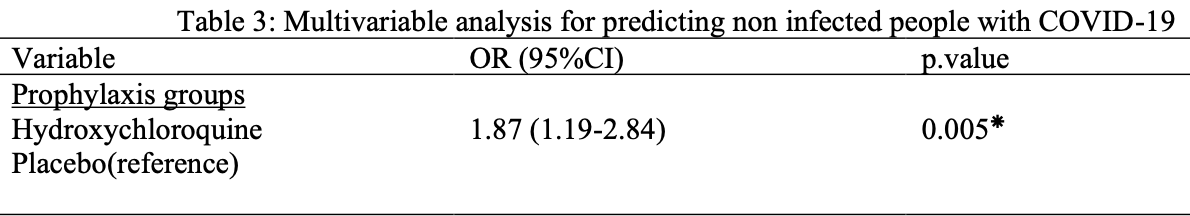
Background: Laboratory and observational data suggest that hydroxychloroquine (HCQ) has biological activity against SARS-CoV-2, potentially permitting its use for disease prevention. This study aimed to evaluate the hydroxychloroquine effect as prophylaxis for SARS-CoV-2 infection. Methods: This double-blind randomized controlled trial was performed on 1000 people between 18-65 who were not suspected of having COVID-19 symptoms at the time of enrollment and had no positive COVID-19 virus test. Hydroxychloroquine or placebo tablets (800 mg/d for the first day followed by 200 mg/d for 6 weeks) were prescribed randomly for participants in 2 groups and followed for 10 weeks. Results: Among 871 participants who were followed within 10 weeks 97(11.1%) became SARS-CoV-2 positive. there were statistically significant differences between infected or noninfected in the hydroxychloroquine (36 of 97 [37.1%]) and placebo (61 of 97 [62.9 %]) groups with a risk ratio of 2.1 (95% confidence interval (CI) 1.01 -3.21; p = 0.005). The incidence of severe forms of COVID-19 (i.e., hospitalized in the coronavirus ward or the ICU) was 2 of 97 (0.02 %) in participants who received a placebo compared to hydroxychloroquine. The proportion of non-infected people who received hydroxychloroquine prophylaxis was nearly twice higher than that of placebo users (1.87, 95% CI: 1.19 -2.84, p = 0.05). There were no significant differences between the two groups regarding side effects (1.1% vs. 0.9%), and no severe adverse reactions were observed.
Conclusion: Pre-exposure therapy with hydroxychloroquine appears to prevent moderate and severe illness caused by COVID-19 in asymptomatic persons.
Author's contribution data analysis and interpretation: Arezoo Chouhdari; statistical analysis: Arezoo Chouhdari; supervision or mentorship: Termeh Tarjoman, Arezoo Chouhdari; write the first draft of the manuscript: Termeh Tarjoman, Arezoo Chouhdari; All authors contributed to the intellectual content, and manuscript editing and read and approved the final manuscript.
Ethical considerations Questionnaires were filled with the participants' satisfaction and written consent was obtained from the participants in this study.
Conflicts of interest All authors declare no conflict of interest.
References
Bansal, Goyal, Cusick, Lahan, Dhaliwal et al., Hydroxychloroquine: a comprehensive review and its controversial role in coronavirus disease 2019, Annals of medicine
Bhatt, Patel, Shah, Parikh, Hydroxychloroquine Prophylaxis against Coronavirus Disease-19: Practice Outcomes among Health-Care Workers, medRxiv
Biot, Daher, Chavain, Fandeur, Khalife et al., Design and synthesis of hydroxyferroquine derivatives with antimalarial and antiviral activities, Journal of medicinal chemistry
Boulware, Pullen, Bangdiwala, Pastick, Lofgren et al., A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19, The New England journal of medicine
Cao, Deng, -X, Dai, Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: An evaluation of the evidence, Travel medicine and infectious disease
Catteau, Dauby, Montourcy, Bottieau, Hautekiet et al., Low-dose hydroxychloroquine therapy and mortality in hospitalised patients with COVID-19: a nationwide observational study of 8075 participants, International journal of antimicrobial agents
Chen, Hu, Zhang, Jiang, Han et al., Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial, medrxiv
Cohen, Hydroxychloroquine for the Prevention of Covid-19 -Searching for Evidence, The New England journal of medicine
Cortegiani, Ippolito, Ingoglia, Iozzo, Giarratano et al., Update I. A systematic review on the efficacy and safety of chloroquine/hydroxychloroquine for COVID-19, Journal of critical care
De Francia, Chiara, COVID-19 Prevention and Treatment, MDPI
Dhibar, Arora, Kakkar, Singla, Mohindra et al., Post-exposure prophylaxis with hydroxychloroquine for the prevention of COVID-19, a myth or a reality? The PEP-CQ Study, International journal of antimicrobial agents
Honein, Rose, Brooks, Meaney-Delman, Cohn, Summary of Guidance for Public Health Strategies to Address High Levels of Community Transmission of SARS-CoV-2 and Related Deaths, December 2020, MMWR Morbidity and mortality weekly report
Horby, Mafham, Linsell, Bell, Staplin et al., Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19, N Engl J Med
Huang, Li, Leung, Liu, Liu et al., A review of therapeutic agents and Chinese herbal medicines against SARS-COV-2 (COVID-19), Pharmacological research
Jung, Kim, Kim, Choi, Chung et al., Effect of hydroxychloroquine preexposure on infection with SARS-CoV-2 in rheumatic disease patients: a population-based cohort study, Clinical Microbiology and Infection
Kashour, Kashour, Gerberi, Tleyjeh, Mortality, viral clearance, and other clinical outcomes of hydroxychloroquine in COVID-19 Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, Clinical and translational science
Khuroo, Chloroquine and hydroxychloroquine in coronavirus disease 2019 (COVID-19). Facts, fiction and the hype: a critical appraisal, International journal of antimicrobial agents
Kloc, Ghobrial, Kubiak, The Role of Genetic Sex and Mitochondria in Response to COVID-19 Infection, International archives of allergy and immunology
Lammers, Brohet, Theunissen, Koster, Rood et al., Early hydroxychloroquine but not chloroquine use reduces ICU admission in COVID-19 patients, International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases
Marmor, Kellner, Lai, Melles, Mieler, Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision), Ophthalmology
Monti, Vertogen, Masini, Donati, Lilli et al., Hydroxychloroquine as prophylaxis for COVID-19: a review, Frontiers in pharmacology
Naggie, Milstone, Castro, Collins, Lakshmi et al., Hydroxychloroquine for pre-exposure prophylaxis of COVID-19 in health care workers: a randomized, multicenter, placebocontrolled trial Healthcare Worker Exposure Response and Outcomes of Hydroxychloroquine (HERO-HCQ), International Journal of Infectious Diseases
Najjar-Debbiny, Gronich, Weber, Khoury, Amar et al., Effectiveness of Paxlovid in reducing severe coronavirus disease 2019 and mortality in high-risk patients, Clinical Infectious Diseases
Panahi, Gorabi, Talaei, Beiraghdar, Akbarzadeh et al., An overview on the treatments and prevention against COVID-19, Virology Journal
Peeri, Shrestha, Rahman, Zaki, Tan et al., The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned?, International journal of epidemiology
Polo, García-Albéniz, Terán, Morales, Rial-Crestelo et al., Daily tenofovir disoproxil fumarate/emtricitabine and hydroxychloroquine for pre-exposure prophylaxis of COVID-19: a double-blind placebo-controlled randomized trial in healthcare workers, Clinical Microbiology and Infection
Pradhan, Olsson, Sex differences in severity and mortality from COVID-19: are males more vulnerable?, Biology of sex differences
Rentsch, Devito, Mackenna, Morton, Bhaskaran et al., Effect of preexposure use of hydroxychloroquine on COVID-19 mortality: a population-based cohort study in patients with rheumatoid arthritis or systemic lupus erythematosus using the OpenSAFELY platform, The Lancet Rheumatology
Ruggieri, Anticoli, 'ambrosio, Giordani, Viora, The influence of sex and gender on immunity, infection and vaccination, Annali dell'Istituto superiore di sanita
Sen, Werner, Shekhar, Within a large healthcare system, the incidence of positive COVID-19 results and mortality are lower in patients on chronic hydroxychloroquine therapy. Drugs & therapy perspectives : for rational drug selection and use
Shabani, Totonchi, Rezaeimirghaed, Gachkar, Hajiesmaeili et al., Evaluation of the prophylactic effect of hydroxychloroquine on people in close-contact with patients with COVID-19, Pulm Pharmacol Ther
Shabani, Totonchi, Rezaeimirghaed, Gachkar, Hajiesmaeili et al., Evaluation of the prophylactic effect of hydroxychloroquine on people in close-contact with patients with COVID-19, Pulmonary Pharmacology & Therapeutics
Smit, Marinosci, Agoritsas, Calmy, Prophylaxis for COVID-19: a systematic review, Clinical microbiology and infection
Wang, Cao, Zhang, Yang, Liu et al., Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro, Cell research
Yao, Ye, Zhang, Cui, Huang et al., In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Clinical infectious diseases : an official publication of the, Infectious Diseases Society of America
DOI record:
{
"DOI": "10.22037/sdh.v10i1.43032",
"ISSN": "2423-7337",
"URL": "https://doi.org/10.22037/sdh.v10i1.43032",
"abstract": "Background: Laboratory and observational data suggest that hydroxychloroquine (HCQ) has biological activity against SARS-CoV-2, potentially permitting its use for disease prevention. This study aimed to evaluate the hydroxychloroquine effect as prophylaxis for SARS-CoV-2 infection. Methods: In this double-blind randomized controlled trial, 1000 healthy people without any signs and symptoms of COVID-19 were randomly assigned in a 1:1 ratio to receive either 800 mg hydroxychloroquine or placebo (four 200 mg tablets in two divided doses on day 1 of the first week, followed by 200 mg (in a single dose) weekly for the next 6 weeks). Results: Among 871 participants who remained and followed within 10 weeks 97(11.1%) became SARS-CoV-2 positive. there were statistically significant differences between infected or non-infected in the hydroxychloroquine (36 of 97 [37.1%]) and placebo (61 of 97 [62.9 %]) groups with a risk ratio of 2.1 (95% confidence interval (CI) 1.01 - 3.21; p = 0.005). The incidence of severe forms of COVID-19 ( hospitalized in the coronavirus ward or the ICU) was 2 of 97 (0.02 %) in participants who received a placebo compared to hydroxychloroquine. The proportion of non-infected people who received hydroxychloroquine prophylaxis was nearly twice higher than that of placebo users (1.87, 95% CI: 1.19 - 2.84, p = 0.05). There were no significant differences between the two groups regarding side effects (1.1% vs. 0.9%), and no severe adverse reactions were observed. Conclusion: Pre-exposure therapy with hydroxychloroquine appears to prevent moderate and severe illness caused by COVID-19 in asymptomatic persons.",
"author": [
{
"family": "Tarjoman",
"given": "Termeh"
},
{
"family": "Valizadeh",
"given": "Mahnaz"
},
{
"family": "Shojaei",
"given": "Parisa"
},
{
"family": "Farhoodi",
"given": "Behnam"
},
{
"family": "Zangeneh",
"given": "Mehrangiz"
},
{
"family": "Najafi",
"given": "Masood"
},
{
"family": "Jamaldini",
"given": "Seyed Hamid"
},
{
"family": "Mesgarian",
"given": "Masoume"
},
{
"family": "Hanifezadeh",
"given": "Zahra"
},
{
"family": "َAbdollahi",
"given": "Faezeh"
},
{
"family": "Massumi Naini",
"given": "Hamidreza"
},
{
"family": "Alijani",
"given": "Mohsen"
},
{
"family": "Ziaee",
"given": "Hasti"
},
{
"family": "Chouhdari",
"given": "Arezoo"
}
],
"container-title": "Social Determinants of Health",
"issue": "Vol. 10 (2024): Continuous Issue",
"issued": {
"date-parts": [
[
2024,
1,
21
]
]
},
"language": "eng",
"medium": "JD",
"publisher": "Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences.",
"publisher-place": "IR",
"title": "The prophylactic effect of hydroxychloroquine on the severity of COVID-19 infection in an asymptomatic population: A randomized clinical trial",
"type": "article-journal",
"volume": "10"
}