Anticoagulant Use in COVID-19 Patients: A Longitudinal Study From Zanjan, Iran
Vanoushe Azimi Pirsaraei, Manizhe Jozpanahi, Koorosh Kamali, Leila Hamzeloo, Seyedeh Pegah Saeid
Cureus, doi:10.7759/cureus.66798
Background The mortality and morbidity of thrombotic events in patients with coronavirus disease 2019 (COVID-19) are increasing worldwide. The clinical impact of prophylactic anticoagulation regimens among these patients in Iran remains unclear. This study aimed to evaluate the use of prophylactic anticoagulants and outcomes among COVID-19 patients admitted to a tertiary referral hospital.
Methodology Patients diagnosed with COVID-19 and hospitalized between March 20 and June 20, 2020, were included in this longitudinal study after obtaining informed consent. Demographic and clinical data were collected from the hospital information system and medical records. Outcomes during this period were also evaluated. The data were entered into the preparation checklist and analyzed using SPSS version 24 software (IBM Corp., Armonk, NY, USA), employing chi-square, Fisher's exact, and Mann-Whitney U tests.
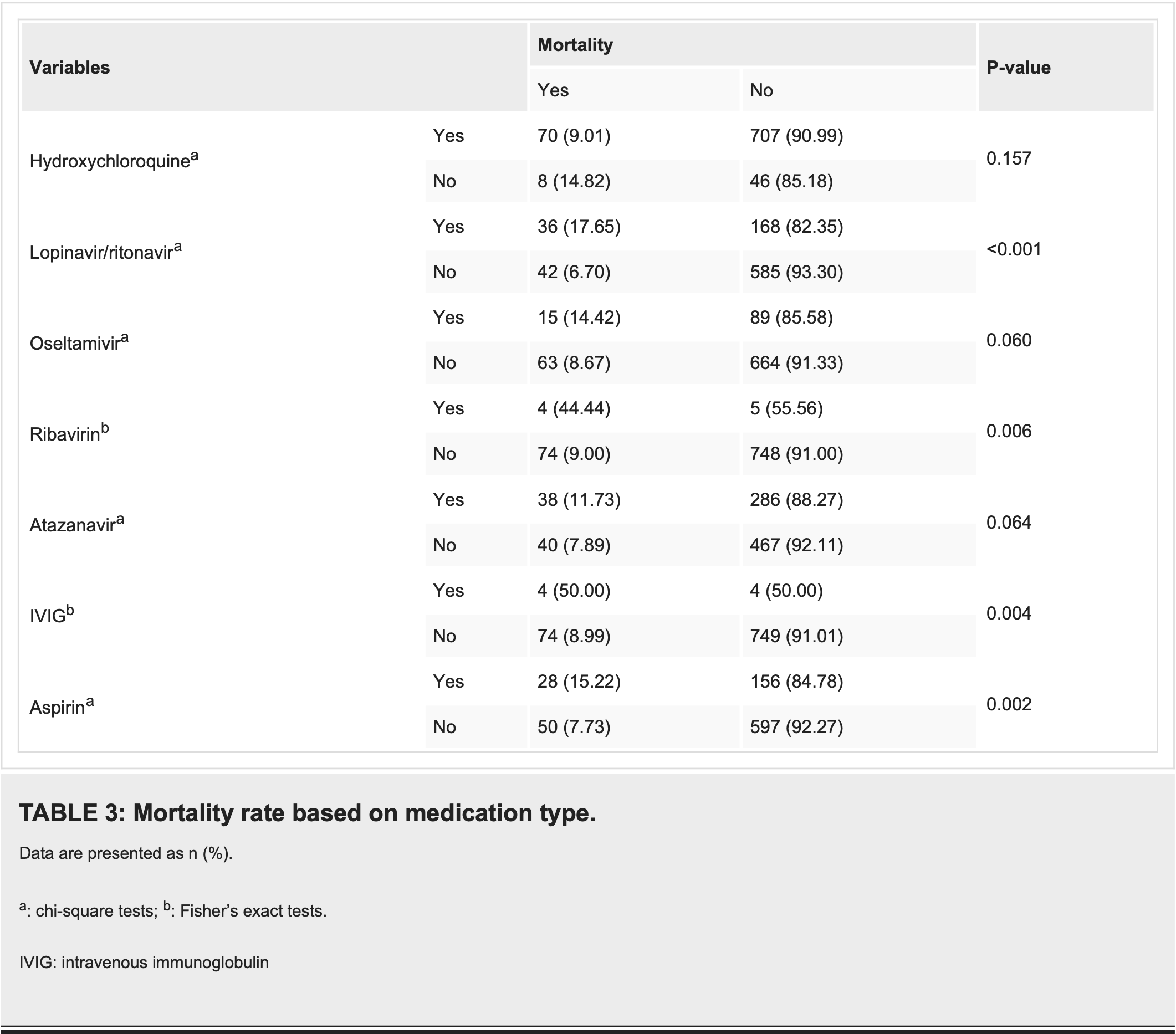
Results Of the 831 enrolled patients, 51.9% were female, and 10.6% needed to be admitted to the intensive care unit (ICU). The mean age of the patients was 57.16 ± 17.32 years, and the mortality rate was estimated to be 9.4%. Mortality rates were significantly higher at older ages, in men, patients with ICU admission, severe pulmonary involvement, malignancy, airway obstruction, ischemic heart disease, and previous cerebrovascular accidents. ICU admission and mortality were statistically significantly higher in those who received concurrent prophylactic anticoagulants and aspirin than in other individuals.
Conclusions Our study demonstrated that administering prophylactic aspirin with or without anticoagulant agents in COVID-19 patients did not reduce mortality rates or ICU transfers. However, it is worth noting that anticoagulant prescription was associated with a decrease in ICU admissions, which could potentially alleviate the significantly higher mortality rates observed among ICU patients in this study. Further research is needed to explore the potential benefits of anticoagulants in COVID-19 treatment.
Additional Information Author Contributions All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work. In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Acquisition, analysis, or interpretation of data
References
Ozma, Maroufi, Khodadadi, Clinical manifestation, diagnosis, prevention and control of SARS-CoV-2 (COVID-19) during the outbreak period, Infez Med
DOI record:
{
"DOI": "10.7759/cureus.66798",
"ISSN": [
"2168-8184"
],
"URL": "http://dx.doi.org/10.7759/cureus.66798",
"author": [
{
"affiliation": [],
"family": "Azimi Pirsaraei",
"given": "Vanoushe",
"sequence": "first"
},
{
"affiliation": [],
"family": "Jozpanahi",
"given": "Manizhe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kamali",
"given": "Koorosh",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hamzeloo",
"given": "Leila",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Saeid",
"given": "Seyedeh Pegah",
"sequence": "additional"
}
],
"container-title": "Cureus",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
13
]
],
"date-time": "2024-08-13T21:49:17Z",
"timestamp": 1723585757000
},
"deposited": {
"date-parts": [
[
2024,
8,
13
]
],
"date-time": "2024-08-13T21:49:24Z",
"timestamp": 1723585764000
},
"indexed": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T00:29:10Z",
"timestamp": 1723595350682
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
8,
13
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.cureus.com/articles/263779-anticoagulant-use-in-covid-19-patients-a-longitudinal-study-from-zanjan-iran",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.7759",
"published": {
"date-parts": [
[
2024,
8,
13
]
]
},
"published-print": {
"date-parts": [
[
2024,
8,
13
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1111/bjh.16727",
"article-title": "Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action",
"author": "Kollias A",
"doi-asserted-by": "publisher",
"journal-title": "Br J Haematol",
"key": "ref1",
"unstructured": "Kollias A, Kyriakoulis KG, Dimakakos E, Poulakou G, Stergiou GS, Syrigos K. Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action. Br J Haematol. 2020, 189:846-7. 10.1111/bjh.16727",
"volume": "189",
"year": "2020"
},
{
"DOI": "10.1007/s11684-020-0767-8",
"article-title": "Coronavirus disease 2019 (COVID-19): a clinical update",
"author": "Zhou M",
"doi-asserted-by": "publisher",
"journal-title": "Front Med",
"key": "ref2",
"unstructured": "Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. 2020, 14:126-35. 10.1007/s11684-020-0767-8",
"volume": "14",
"year": "2020"
},
{
"article-title": "Clinical manifestation, diagnosis, prevention and control of SARS-CoV-2 (COVID-19) during the outbreak period",
"author": "Ozma MA",
"journal-title": "Infez Med",
"key": "ref3",
"unstructured": "Ozma MA, Maroufi P, Khodadadi E, et al.. Clinical manifestation, diagnosis, prevention and control of SARS-CoV-2 (COVID-19) during the outbreak period. Infez Med. 2020, 28:153-65.",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.04.031",
"article-title": "COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review",
"author": "Bikdeli B",
"doi-asserted-by": "publisher",
"journal-title": "J Am Coll Cardiol",
"key": "ref4",
"unstructured": "Bikdeli B, Madhavan MV, Jimenez D, et al.. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020, 75:2950-73. 10.1016/j.jacc.2020.04.031",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1007/s11239-020-02125-4",
"article-title": "Venous thromboembolism and heparin use in COVID-19 patients: juggling between pragmatic choices, suggestions of medical societies and the lack of guidelines",
"author": "Porfidia A",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Thrombolysis",
"key": "ref5",
"unstructured": "Porfidia A, Pola R. Venous thromboembolism and heparin use in COVID-19 patients: juggling between pragmatic choices, suggestions of medical societies and the lack of guidelines. J Thromb Thrombolysis. 2020, 50:68-71. 10.1007/s11239-020-02125-4",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00607-2020",
"article-title": "Pathogenesis of COVID-19 from a cell biology perspective",
"author": "Mason RJ",
"doi-asserted-by": "publisher",
"journal-title": "Eur Respir J",
"key": "ref6",
"unstructured": "Mason RJ. Pathogenesis of COVID-19 from a cell biology perspective. Eur Respir J. 2020, 55:2000607. 10.1183/13993003.00607-2020",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2020.109975",
"article-title": "Should aspirin be used for prophylaxis of COVID-19-induced coagulopathy?",
"author": "Mohamed-Hussein AA",
"doi-asserted-by": "publisher",
"journal-title": "Med Hypotheses",
"key": "ref7",
"unstructured": "Mohamed-Hussein AA, Aly KM, Ibrahim MA. Should aspirin be used for prophylaxis of COVID-19-induced coagulopathy?. Med Hypotheses. 2020, 144:109975. 10.1016/j.mehy.2020.109975",
"volume": "144",
"year": "2020"
},
{
"DOI": "10.1007/s11239-020-02138-z",
"article-title": "Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum",
"author": "Barnes GD",
"doi-asserted-by": "publisher",
"journal-title": "J Thromb Thrombolysis",
"key": "ref8",
"unstructured": "Barnes GD, Burnett A, Allen A, et al.. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020, 50:72-81. 10.1007/s11239-020-02138-z",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1007/s00134-020-06062-x",
"article-title": "High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study",
"author": "Helms J",
"doi-asserted-by": "publisher",
"journal-title": "Intensive Care Med",
"key": "ref9",
"unstructured": "Helms J, Tacquard C, Severac F, et al.. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020, 46:1089-98. 10.1007/s00134-020-06062-x",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.04.013",
"article-title": "Incidence of thrombotic complications in critically ill ICU patients with COVID-19",
"author": "Klok FA",
"doi-asserted-by": "publisher",
"journal-title": "Thromb Res",
"key": "ref10",
"unstructured": "Klok FA, Kruip MJ, van der Meer NJ, et al.. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020, 191:145-7. 10.1016/j.thromres.2020.04.013",
"volume": "191",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.551889",
"article-title": "Iran's approach to COVID-19: evolving treatment protocols and ongoing clinical trials",
"author": "Rahmanzade R",
"doi-asserted-by": "publisher",
"journal-title": "Front Public Health",
"key": "ref11",
"unstructured": "Rahmanzade R, Rahmanzadeh R, Hashemian SM, Tabarsi P. Iran's approach to COVID-19: evolving treatment protocols and ongoing clinical trials. Front Public Health. 2020, 8:551889. 10.3389/fpubh.2020.551889",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1155/2021/6697677",
"article-title": "Correlation between chest CT severity scores and the clinical parameters of adult patients with COVID-19 pneumonia",
"author": "Saeed GA",
"doi-asserted-by": "publisher",
"journal-title": "Radiol Res Pract",
"key": "ref12",
"unstructured": "Saeed GA, Gaba W, Shah A, et al.. Correlation between chest CT severity scores and the clinical parameters of adult patients with COVID-19 pneumonia. Radiol Res Pract. 2021, 2021:6697677. 10.1155/2021/6697677",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1016/j.cca.2020.05.044",
"article-title": "COVID-19: transmission, prevention, and potential therapeutic opportunities",
"author": "Lotfi M",
"doi-asserted-by": "publisher",
"journal-title": "Clin Chim Acta",
"key": "ref13",
"unstructured": "Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020, 508:254-66. 10.1016/j.cca.2020.05.044",
"volume": "508",
"year": "2020"
},
{
"DOI": "10.1016/j.jamda.2020.05.045",
"article-title": "The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects",
"author": "Bonanad C",
"doi-asserted-by": "publisher",
"journal-title": "J Am Med Dir Assoc",
"key": "ref14",
"unstructured": "Bonanad C, García-Blas S, Tarazona-Santabalbina F, et al.. The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 2020, 21:915-8. 10.1016/j.jamda.2020.05.045",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1186/s13293-020-00330-7",
"article-title": "Sex differences in severity and mortality from COVID-19: are males more vulnerable?",
"author": "Pradhan A",
"doi-asserted-by": "publisher",
"journal-title": "Biol Sex Differ",
"key": "ref15",
"unstructured": "Pradhan A, Olsson PE. Sex differences in severity and mortality from COVID-19: are males more vulnerable?. Biol Sex Differ. 2020, 11:53. 10.1186/s13293-020-00330-7",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.34172/aim.2020.102",
"article-title": "Clinical characteristics and outcomes of 905 COVID-19 patients admitted to Imam Khomeini Hospital Complex in the capital city of Tehran, Iran",
"author": "Allameh SF",
"doi-asserted-by": "publisher",
"journal-title": "Arch Iran Med",
"key": "ref16",
"unstructured": "Allameh SF, Nemati S, Ghalehtaki R, et al.. Clinical characteristics and outcomes of 905 COVID-19 patients admitted to Imam Khomeini Hospital Complex in the capital city of Tehran, Iran. Arch Iran Med. 2020, 23:766-75. 10.34172/aim.2020.102",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2021.100789",
"article-title": "COPD and the risk of poor outcomes in COVID-19: a systematic review and meta-analysis",
"author": "Gerayeli FV",
"doi-asserted-by": "publisher",
"journal-title": "EClinicalMedicine",
"key": "ref17",
"unstructured": "Gerayeli FV, Milne S, Cheung C, et al.. COPD and the risk of poor outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021, 33:100789. 10.1016/j.eclinm.2021.100789",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.23750/abm.v92i3.10630",
"article-title": "Predictors of clinical outcomes in adult COVID-19 patients admitted to a tertiary care hospital in India: an analytical cross-sectional study",
"author": "Chauhan NK",
"doi-asserted-by": "publisher",
"journal-title": "Acta Biomed",
"key": "ref18",
"unstructured": "Chauhan NK, Shadrach BJ, Garg MK, et al.. Predictors of clinical outcomes in adult COVID-19 patients admitted to a tertiary care hospital in India: an analytical cross-sectional study. Acta Biomed. 2021, 92:e2021024. 10.23750/abm.v92i3.10630",
"volume": "92",
"year": "2021"
},
{
"DOI": "10.1093/jac/dkaa403",
"article-title": "Efficacy of chloroquine or hydroxychloroquine in COVID-19 patients: a systematic review and meta-analysis",
"author": "Kashour Z",
"doi-asserted-by": "publisher",
"journal-title": "J Antimicrob Chemother",
"key": "ref19",
"unstructured": "Kashour Z, Riaz M, Garbati MA, et al.. Efficacy of chloroquine or hydroxychloroquine in COVID-19 patients: a systematic review and meta-analysis. J Antimicrob Chemother. 2021, 76:30-42. 10.1093/jac/dkaa403",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1080/14787210.2021.1848545",
"article-title": "Efficacy and safety of lopinavir/ritonavir in the treatment of COVID-19: a systematic review",
"author": "Joseph BA",
"doi-asserted-by": "publisher",
"journal-title": "Expert Rev Anti Infect Ther",
"key": "ref20",
"unstructured": "Joseph BA, Dibas M, Evanson KW, et al.. Efficacy and safety of lopinavir/ritonavir in the treatment of COVID-19: a systematic review. Expert Rev Anti Infect Ther. 2021, 19:679-87. 10.1080/14787210.2021.1848545",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1101/2020.07.20.20157891",
"article-title": "Intravenous immunoglobulin (IVIG) significantly reduces respiratory morbidity in COVID-19 pneumonia: a prospective randomized trial",
"author": "Sakoulas G",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "ref21",
"unstructured": "Sakoulas G, Geriak M, Kullar R, et al.. Intravenous immunoglobulin (IVIG) significantly reduces respiratory morbidity in COVID-19 pneumonia: a prospective randomized trial. medRxiv. 2020, 10.1101/2020.07.20.20157891",
"year": "2020"
},
{
"DOI": "10.1016/j.intimp.2020.107205",
"article-title": "Evaluating the effects of intravenous immunoglobulin (IVIg) on the management of severe COVID-19 cases: a randomized controlled trial",
"author": "Tabarsi P",
"doi-asserted-by": "publisher",
"journal-title": "Int Immunopharmacol",
"key": "ref22",
"unstructured": "Tabarsi P, Barati S, Jamaati H, et al.. Evaluating the effects of intravenous immunoglobulin (IVIg) on the management of severe COVID-19 cases: a randomized controlled trial. Int Immunopharmacol. 2021, 90:107205. 10.1016/j.intimp.2020.107205",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.3390/medicina57090931",
"article-title": "Aspirin is related to worse clinical outcomes of COVID-19",
"author": "Kim I",
"doi-asserted-by": "publisher",
"journal-title": "Medicina (Kaunas)",
"key": "ref23",
"unstructured": "Kim I, Yoon S, Kim M, Lee H, Park S, Kim W, Lee S. Aspirin is related to worse clinical outcomes of COVID-19. Medicina (Kaunas). 2021, 57:931. 10.3390/medicina57090931",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1161/JAHA.121.024530",
"article-title": "Aspirin therapy on prophylactic anticoagulation for patients hospitalized with COVID-19: a propensity score-matched cohort analysis of the HOPE-COVID-19 Registry",
"author": "Santoro F",
"doi-asserted-by": "publisher",
"journal-title": "J Am Heart Assoc",
"key": "ref24",
"unstructured": "Santoro F, Núñez-Gil IJ, Vitale E, et al.. Aspirin therapy on prophylactic anticoagulation for patients hospitalized with COVID-19: a propensity score-matched cohort analysis of the HOPE-COVID-19 Registry. J Am Heart Assoc. 2022, 11:e024530. 10.1161/JAHA.121.024530",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1136/openhrt-2021-001785",
"article-title": "Combined anticoagulant and antiplatelet therapy is associated with an improved outcome in hospitalised patients with COVID-19: a propensity matched cohort study",
"author": "Matli K",
"doi-asserted-by": "publisher",
"journal-title": "Open Heart",
"key": "ref25",
"unstructured": "Matli K, Chamoun N, Fares A, et al.. Combined anticoagulant and antiplatelet therapy is associated with an improved outcome in hospitalised patients with COVID-19: a propensity matched cohort study. Open Heart. 2021, 8:e001785. 10.1136/openhrt-2021-001785",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1007/s15010-022-01809-8",
"article-title": "Efficacy of different anticoagulant doses for patients with COVID-19: a systematic review and network meta-analysis",
"author": "Yasuda H",
"doi-asserted-by": "publisher",
"journal-title": "Infection",
"key": "ref26",
"unstructured": "Yasuda H, Mayumi T, Okano H. Efficacy of different anticoagulant doses for patients with COVID-19: a systematic review and network meta-analysis. Infection. 2022, 50:1453-63. 10.1007/s15010-022-01809-8",
"volume": "50",
"year": "2022"
},
{
"DOI": "10.1016/j.cmi.2020.07.030",
"article-title": "CT lung lesions as predictors of early death or ICU admission in COVID-19 patients",
"author": "Ruch Y",
"doi-asserted-by": "publisher",
"journal-title": "Clin Microbiol Infect",
"key": "ref27",
"unstructured": "Ruch Y, Kaeuffer C, Ohana M, et al.. CT lung lesions as predictors of early death or ICU admission in COVID-19 patients. Clin Microbiol Infect. 2020, 26:1417.e5-8. 10.1016/j.cmi.2020.07.030",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0244171",
"article-title": "Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru",
"author": "Mejía F",
"doi-asserted-by": "publisher",
"journal-title": "PLoS One",
"key": "ref28",
"unstructured": "Mejía F, Medina C, Cornejo E, et al.. Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru. PLoS One. 2020, 15:e0244171. 10.1371/journal.pone.0244171",
"volume": "15",
"year": "2020"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.cureus.com/articles/263779-anticoagulant-use-in-covid-19-patients-a-longitudinal-study-from-zanjan-iran"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Anticoagulant Use in COVID-19 Patients: A Longitudinal Study From Zanjan, Iran",
"type": "journal-article"
}